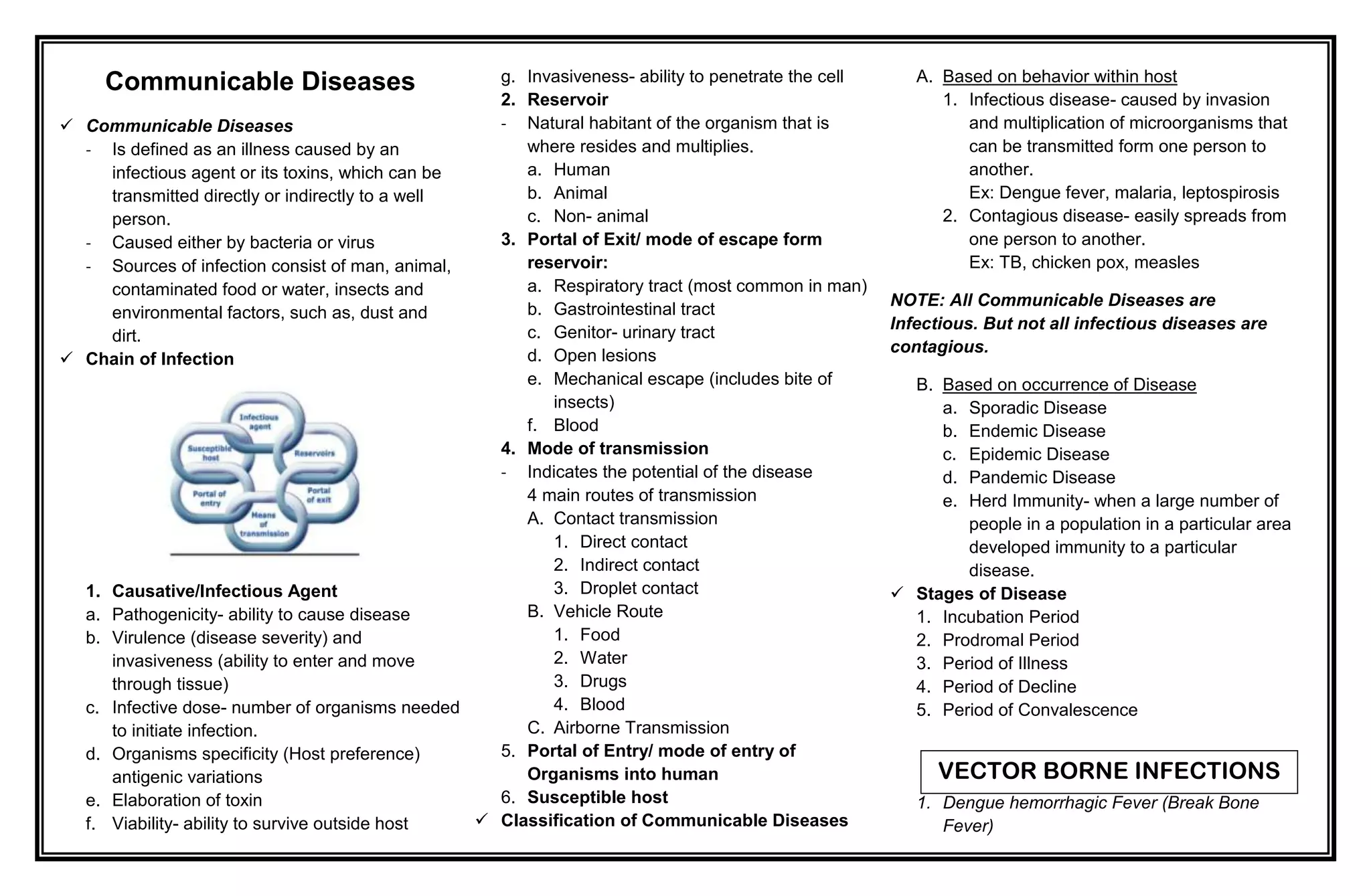
This document discusses communicable diseases and central nervous system infections. It defines communicable diseases and outlines the chain of infection, including the infectious agent, reservoir, mode of transmission, portal of entry/exit, and susceptible host. It also classifies diseases based on occurrence and stages of disease. Specific diseases discussed include dengue fever, malaria, filariasis, meningitis, meningococcemia, and rabies. Treatment and nursing considerations are provided for each condition.