Colon cancer is the third most common malignancy worldwide. It typically presents in individuals over 50 years of age with symptoms like weight loss, anemia, abdominal discomfort, and rectal bleeding. Diagnosis involves blood tests, imaging like CT scan to evaluate the colon and detect metastasis, and colonoscopy to directly visualize the colon and perform biopsies. Staging uses the TNM system and determines appropriate treatment and prognosis.









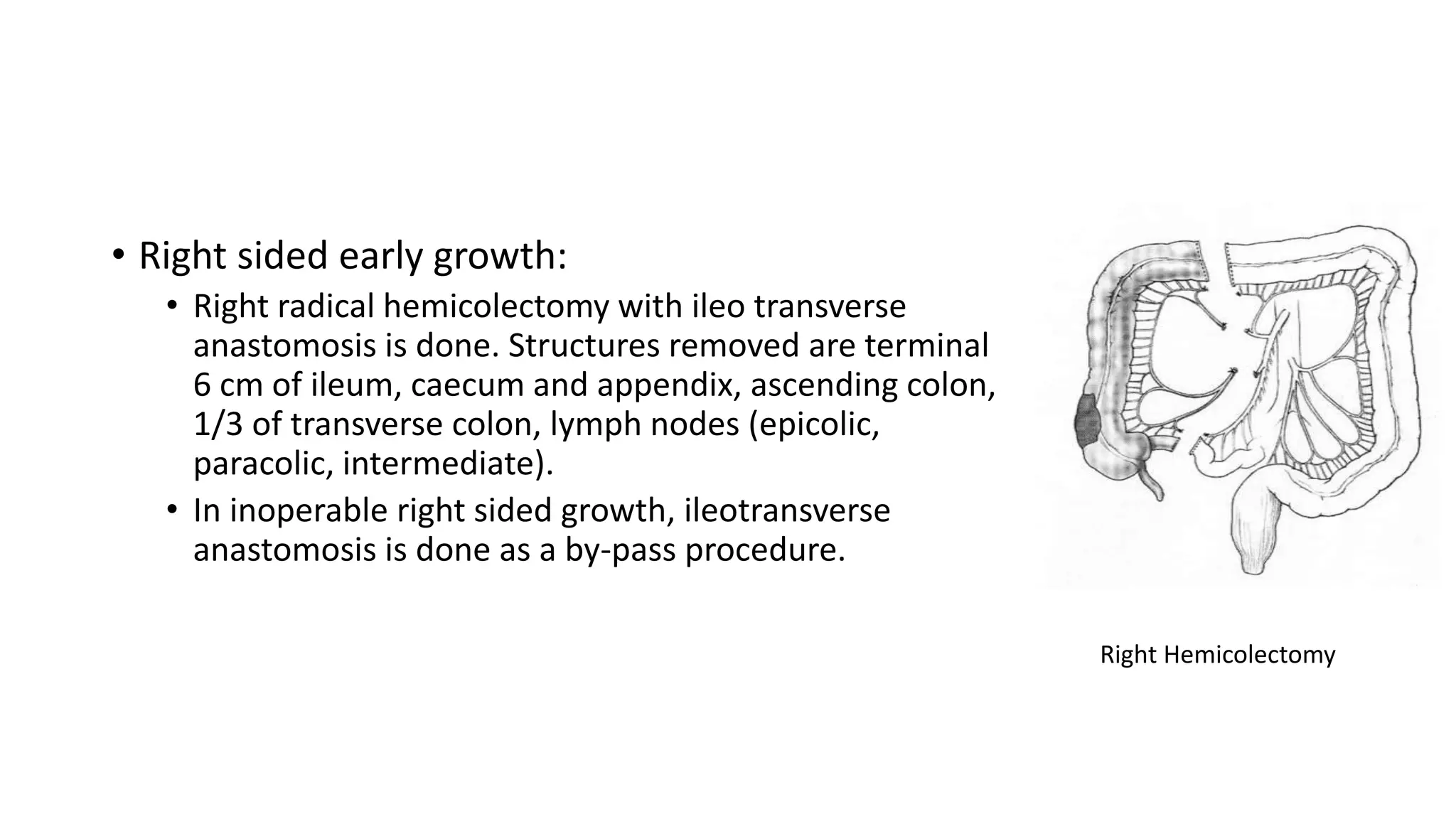
![Pathogenesis
• Adenoma—carcinoma sequence
• Most of the colonic carcinoma develops from polyp/adenoma pathway.
• Normal epithelium →initiation by 5q loss APC gene →dysplasia (hyperproliferative) → DNA methylation
→early adenoma → 12p activation K ras → intermediate adenoma →18q loss DCC → late adenoma → action
by 17p loss p53 →carcinoma → spread .
• 80% of colorectal cancer arises from loss of heterozygosity (LOH) pathway.
• LOH pathway is due to APC gene defects (in FAP), K ras mutation altering the cell cycle [K ras binds to GTP
(guanosine triphosphate) hydrolyse to GDP which inactivates G protein normally; K ras mutation blocks GTP
hydrolyse leading into permanently active form of G protein causing carcinoma]; loss of DCC tumour
suppressor gene; mutation of tumour suppressor gene p53. LOH pathway is microsatellite stable (MSS) and
carries poor prognosis compared with MSI
• 20% of colorectal cancer develops from mutation from RER (Replication Error Repair) pathway wherein
repair mechanism of DNA replication error is lost. It causes microsatellite regions of genome to have
repeated sequences leading into error and is called as microsatellite instability (MSI). In colon, it is seen in
right side growths and is associated with better prognosis.](https://image.slidesharecdn.com/coloncancer-201021092519/75/Colon-cancer-11-2048.jpg)