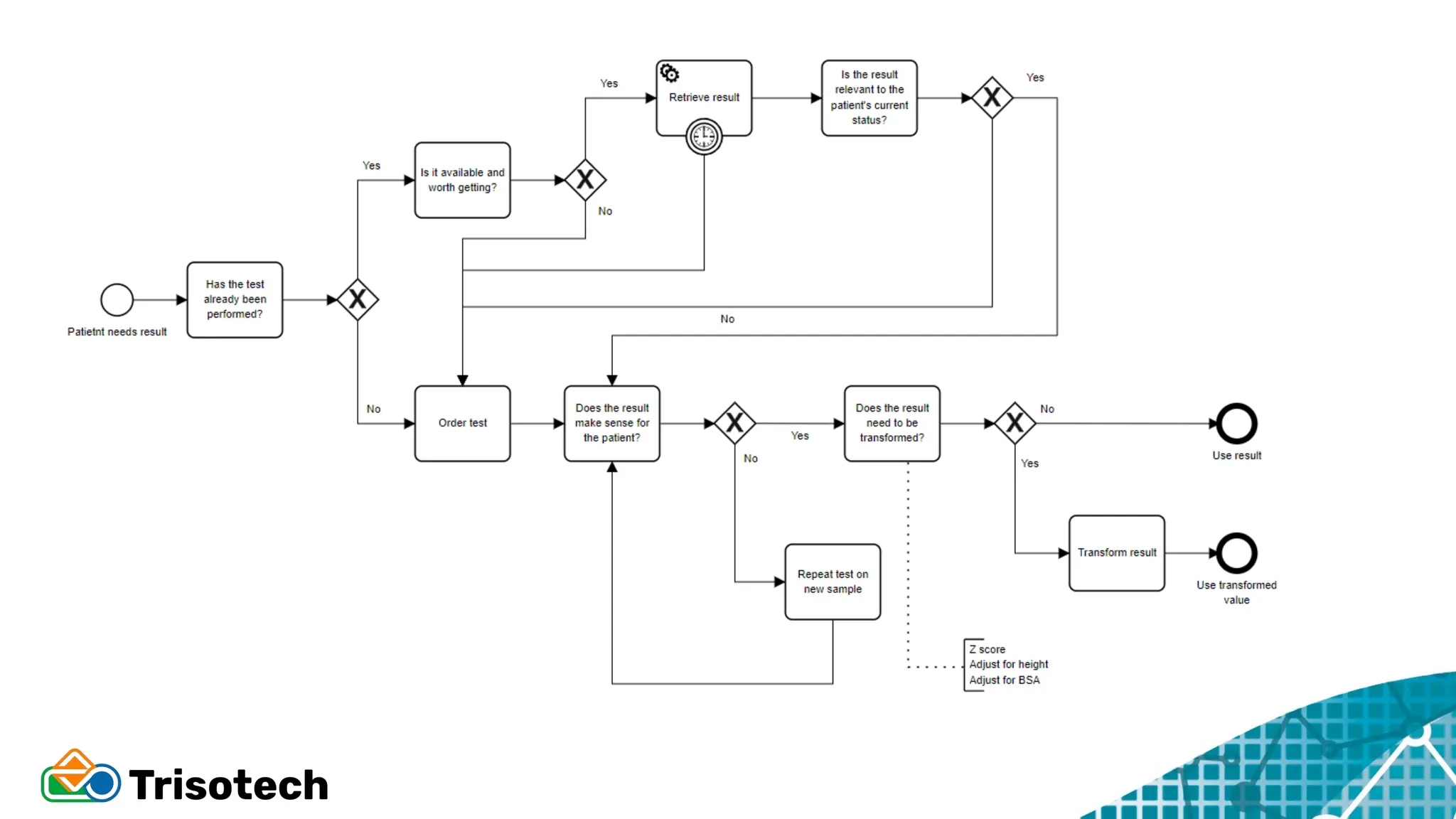
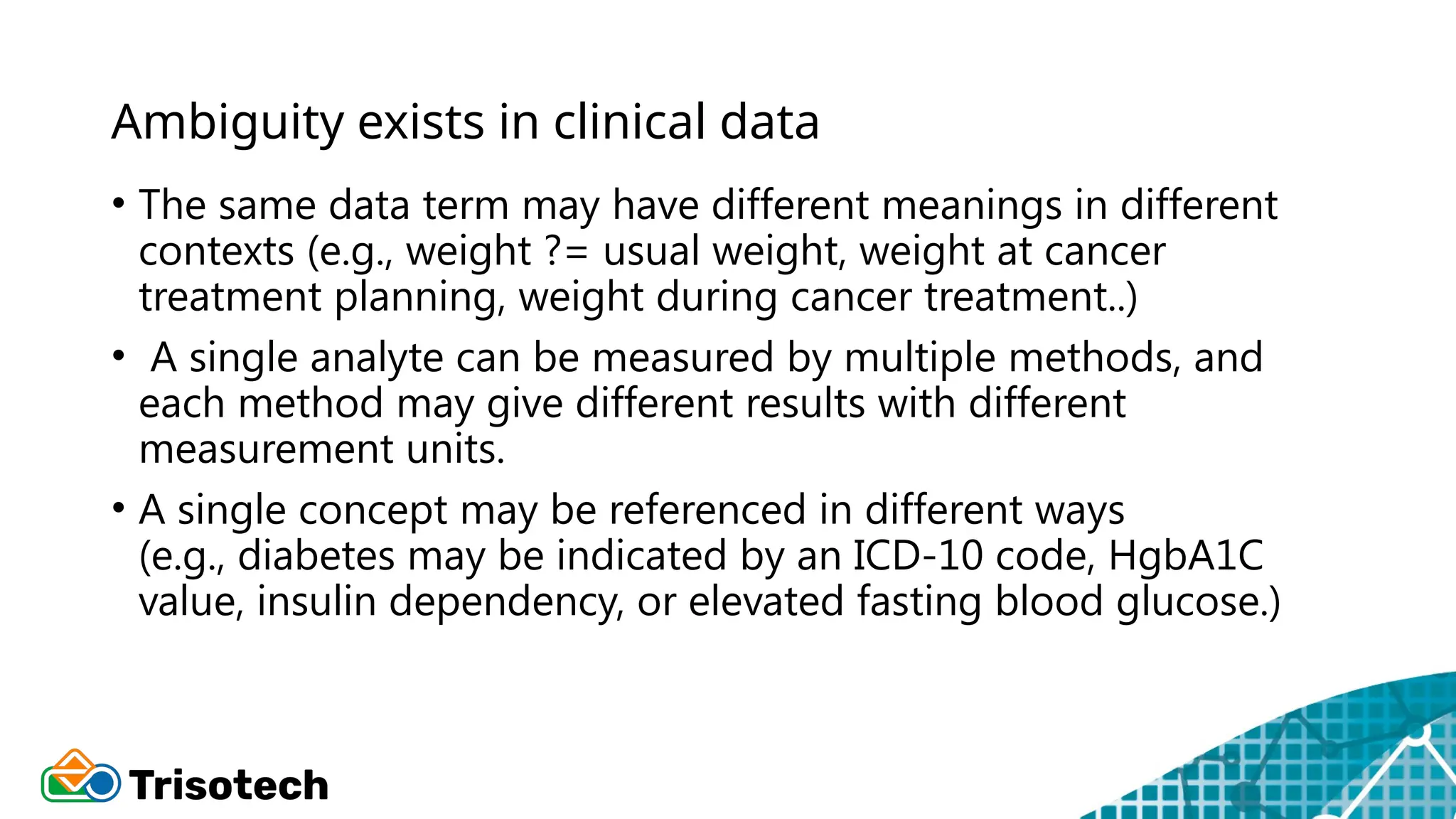
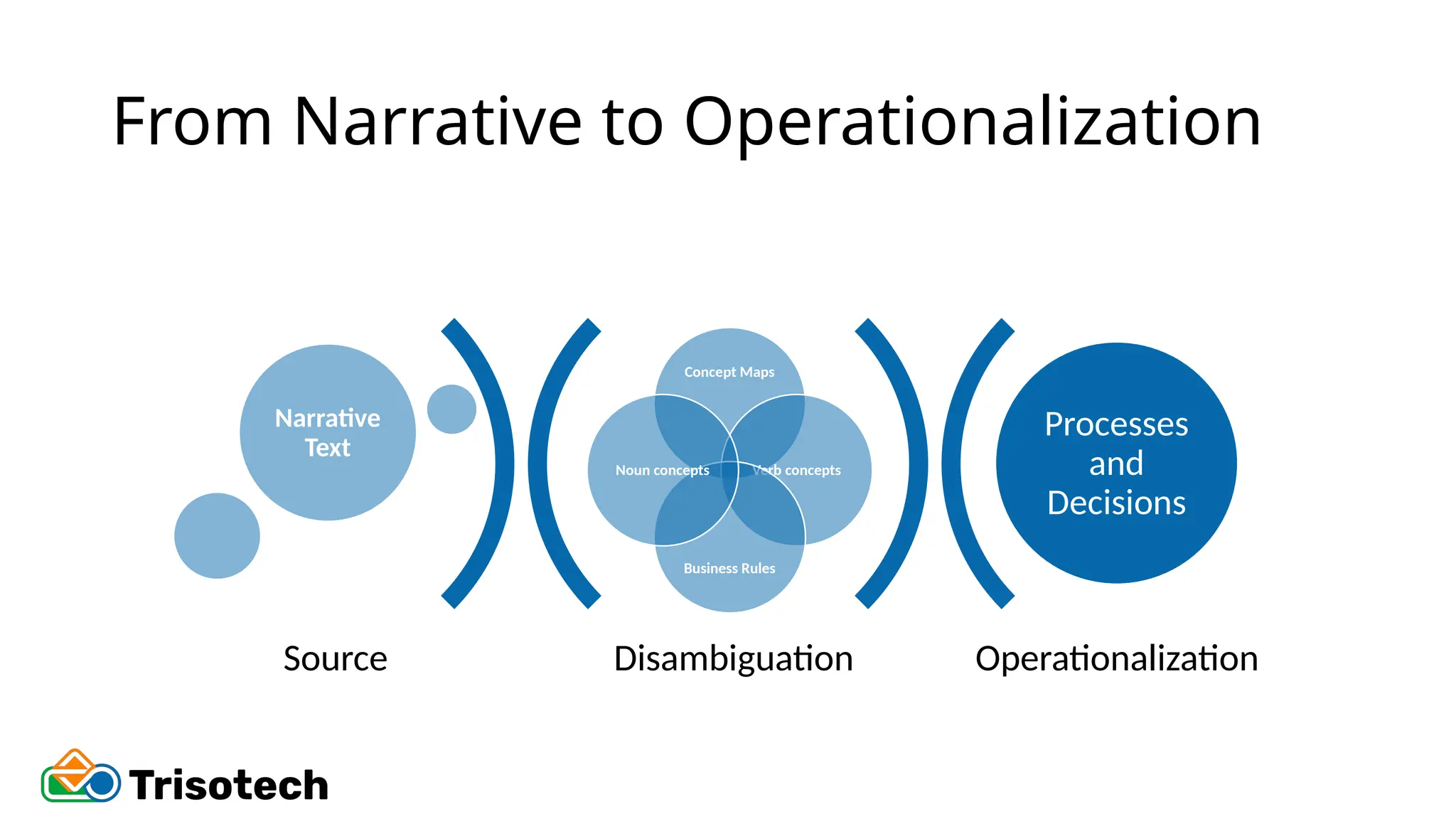
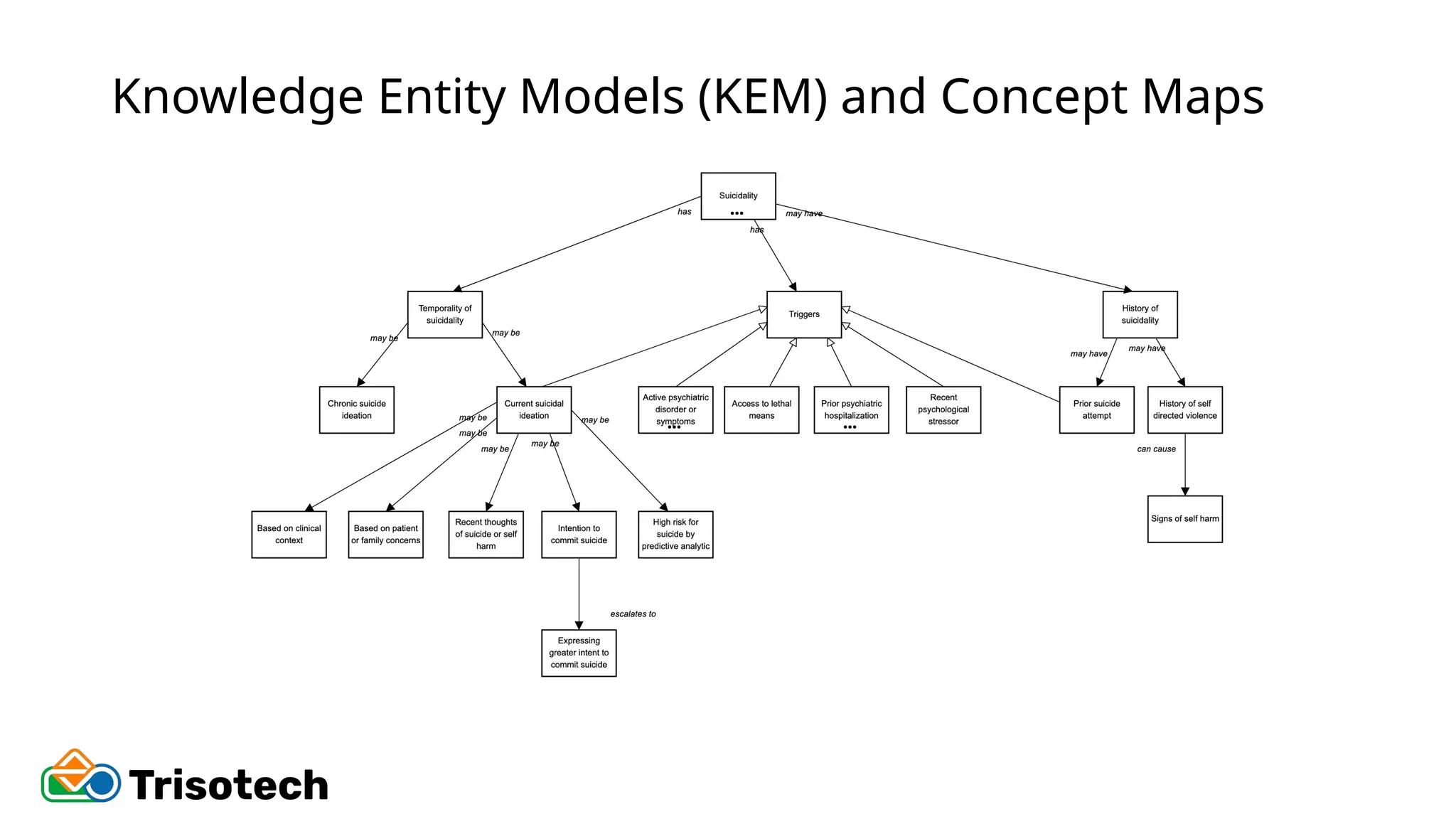
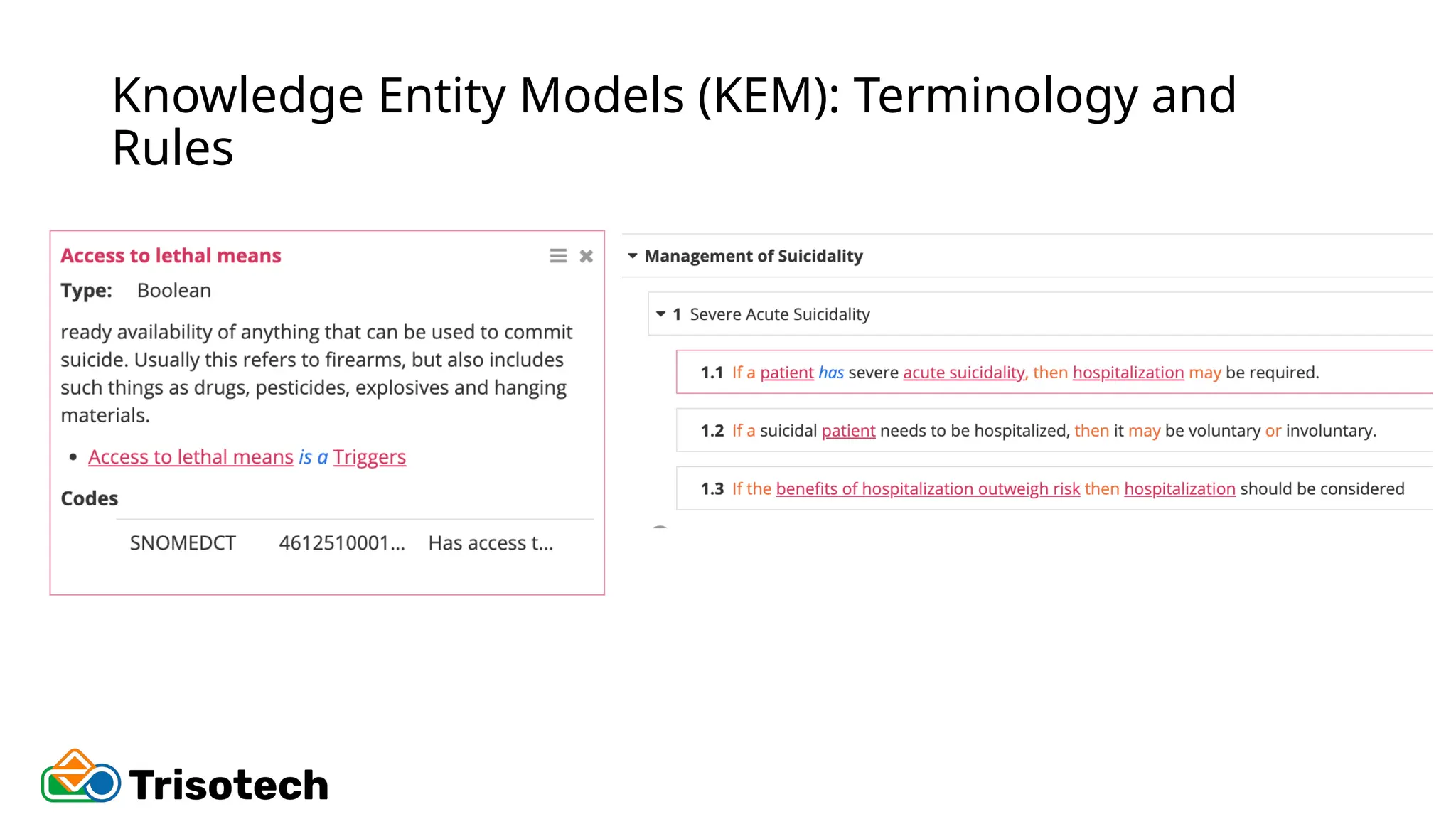
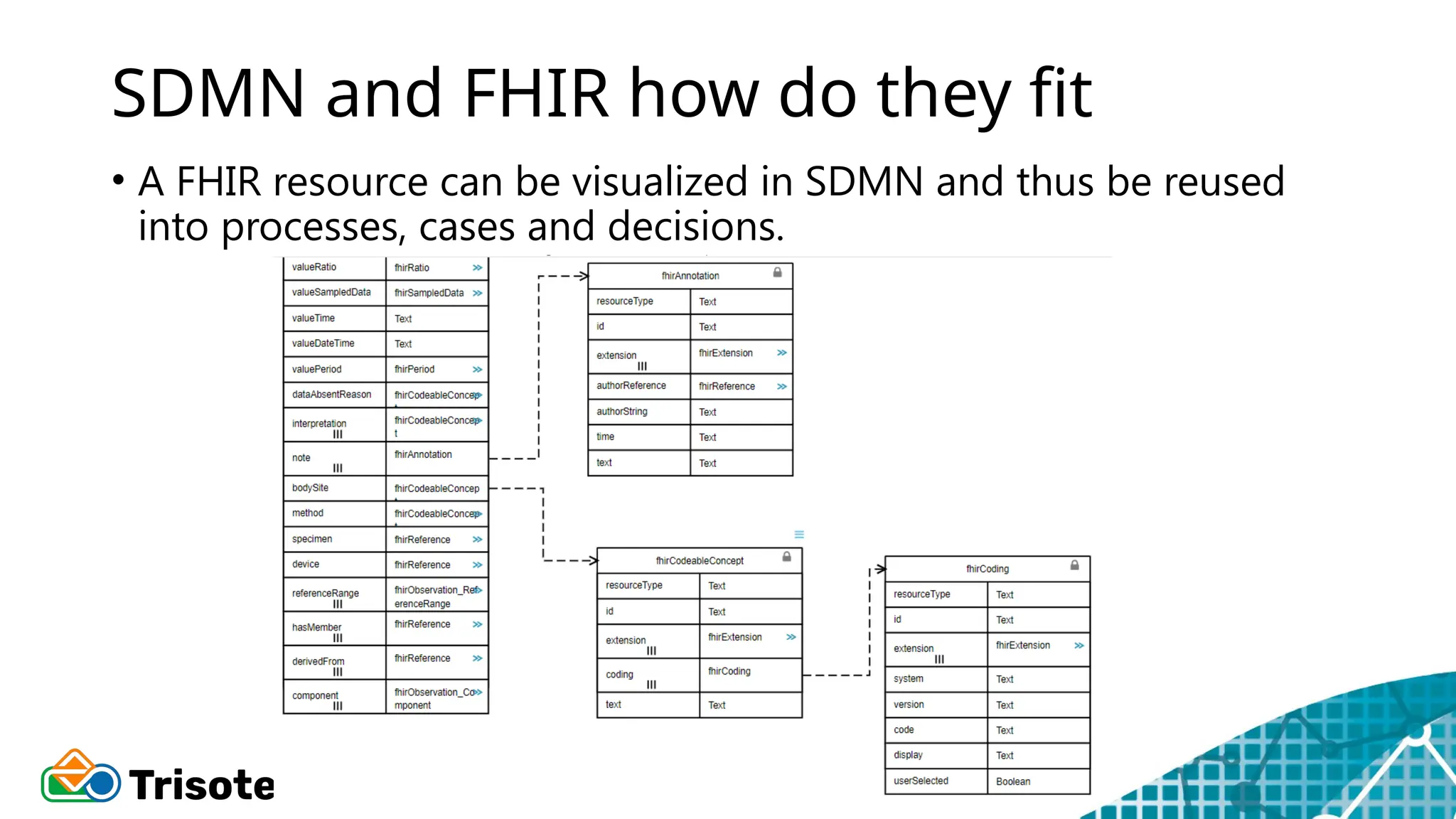
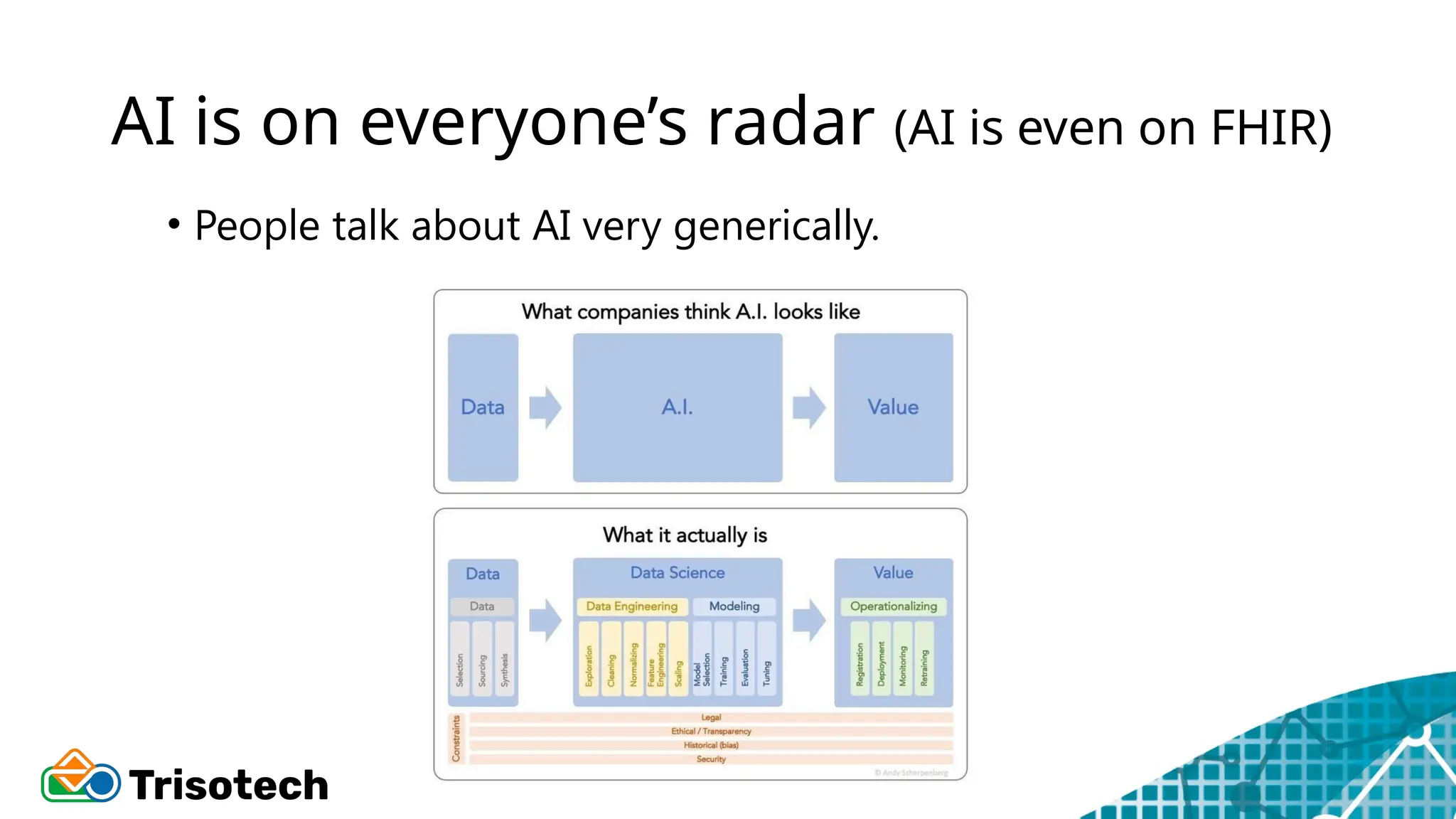
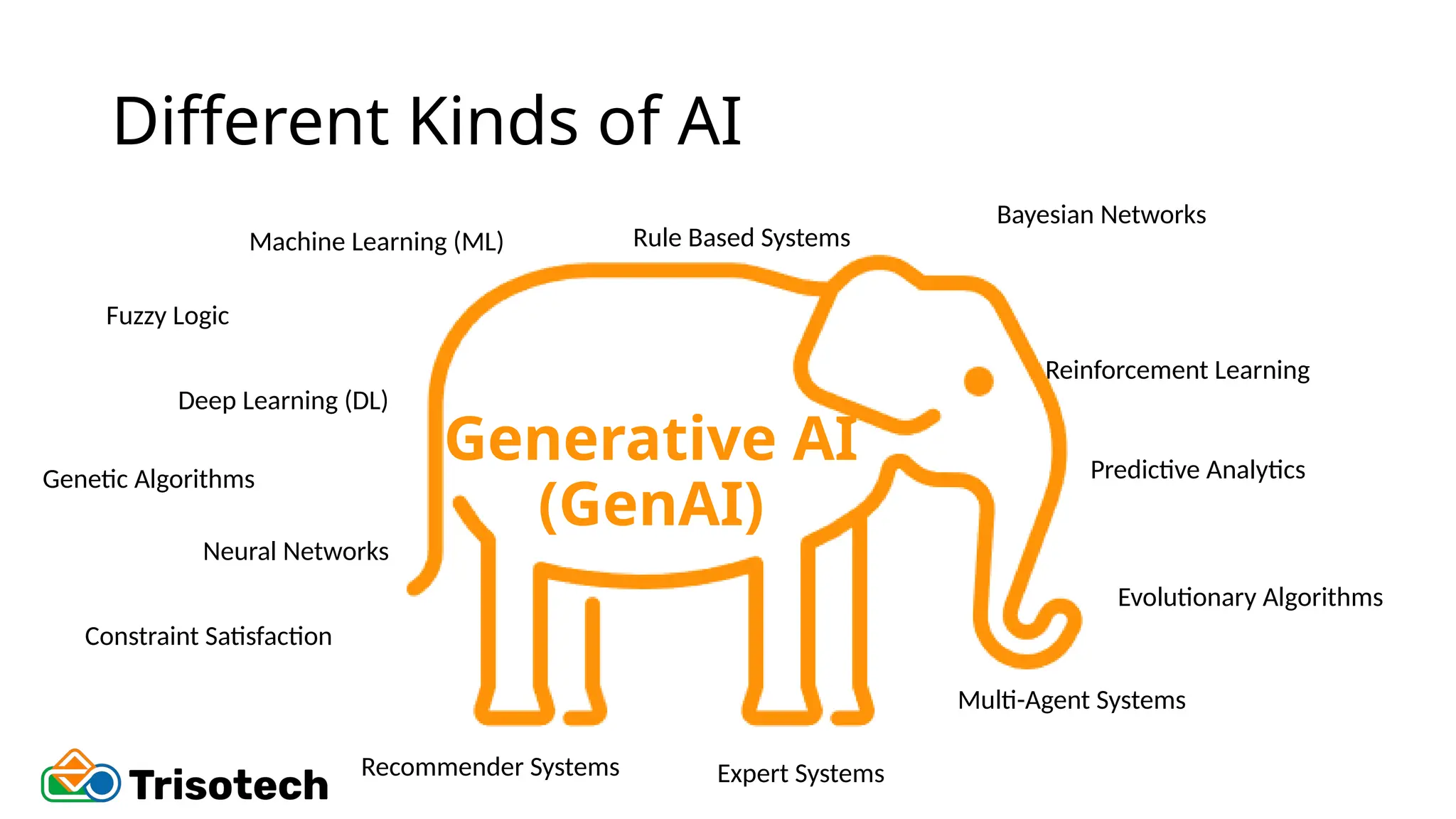
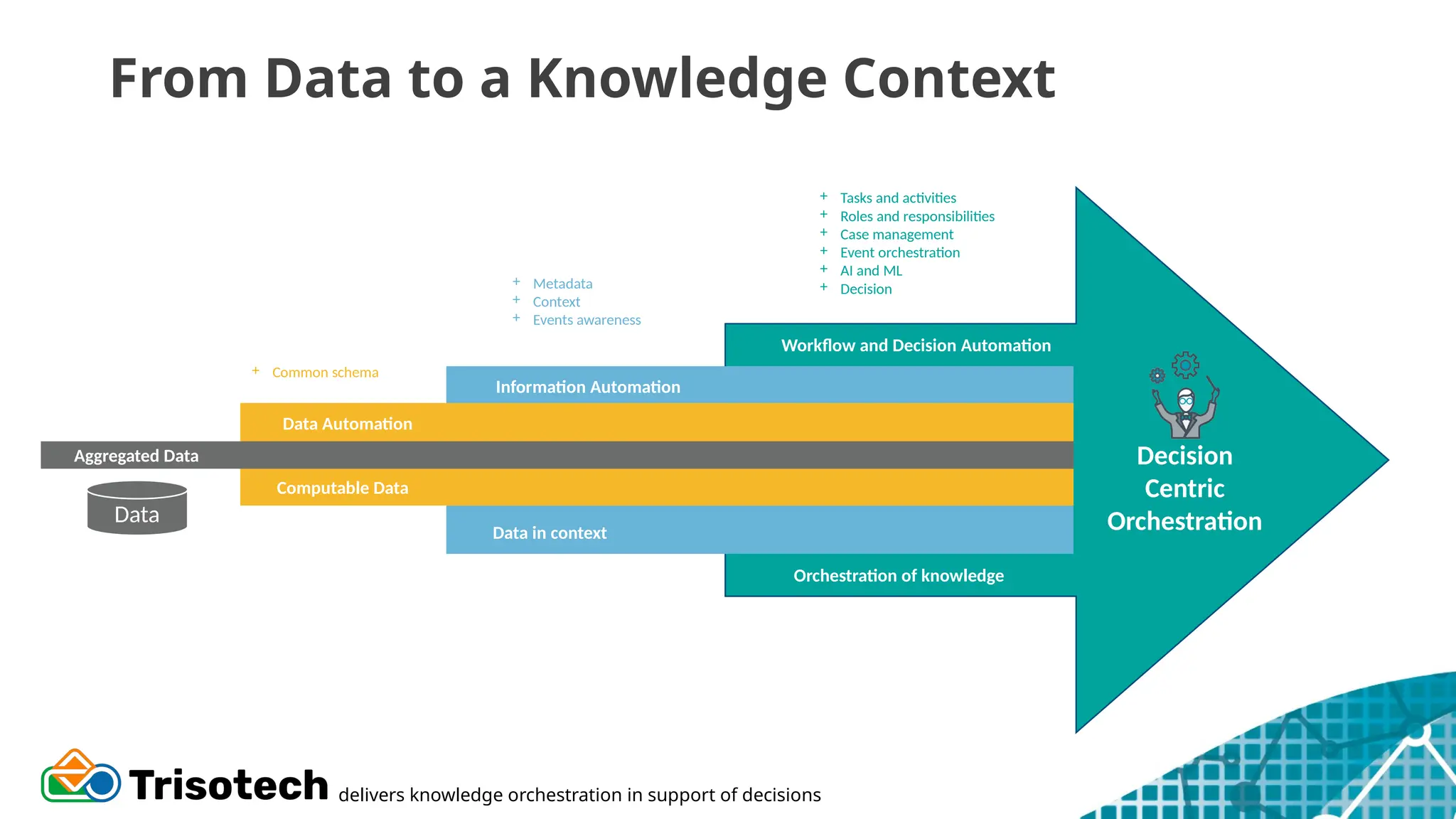
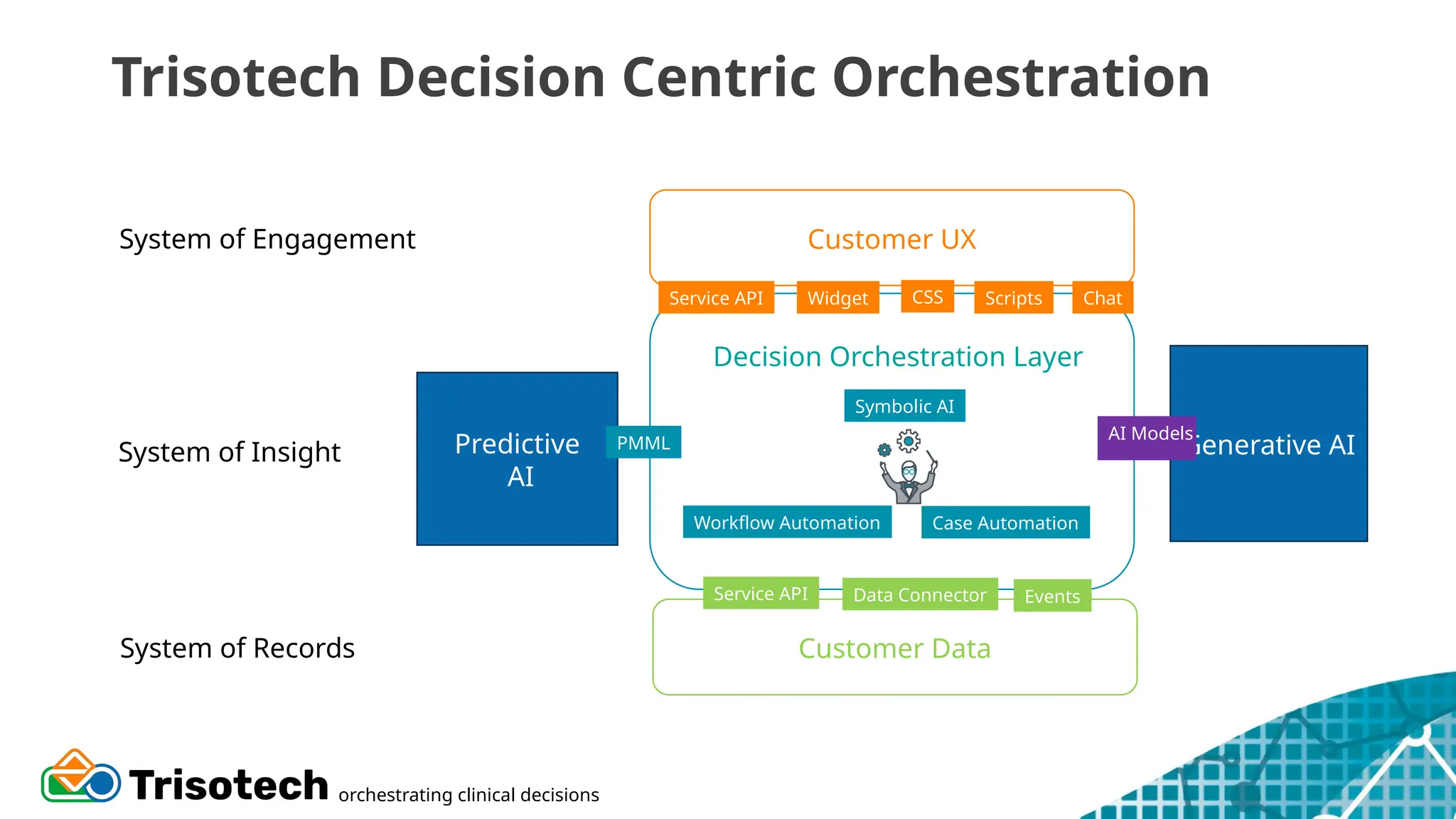
The document discusses the integration of clinician-centric data and AI in healthcare decision-making, emphasizing the importance of structured, clean data to improve patient outcomes. It explores clinician thought processes when accessing data, challenges with ambiguity in clinical data, and the need for interoperability through standards like FHIR and SDMN. Additionally, it addresses the role of AI in enhancing healthcare delivery, highlighting the necessity of data cleansing and efficient data management.