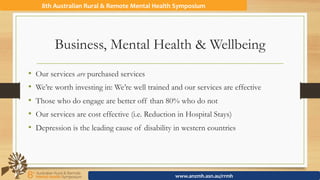
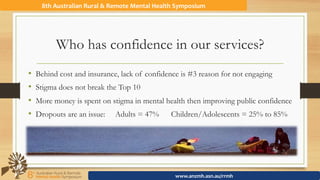
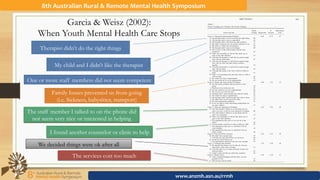
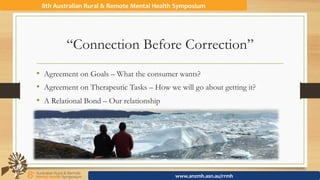
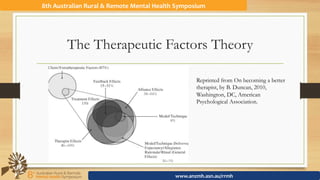
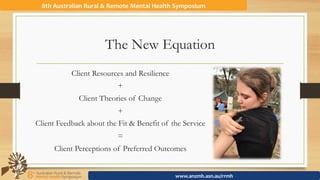
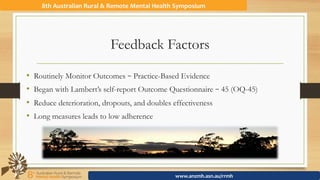
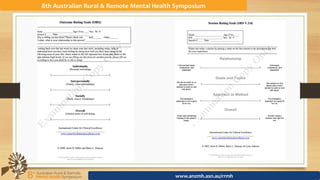
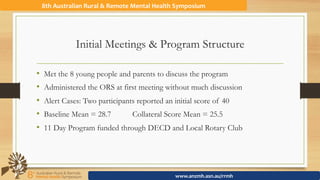
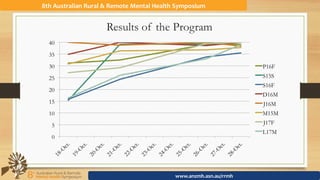
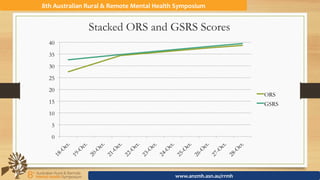
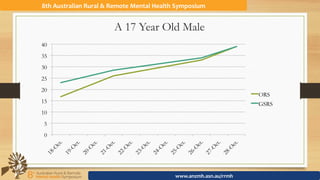
The document discusses the importance of consumer-driven, recovery-oriented practices in mental health, emphasizing feedback-informed treatment to enhance consumer participation. It outlines various factors that influence engagement in mental health services and critiques traditional therapeutic relationships, advocating for a relational bond between clients and therapists. The presentation also highlights the need for continuous quality improvement and empirical support for treatment effectiveness through client feedback.








![My Name is Will & I’m a Social Worker
Education
BSW - University of Maryland – Baltimore County
MSW[AP] - Charles Sturt University
v
Run a small adventure therapy program in SA
Awarded Australian Postgraduate Award by CSU
Australian Association for Bush Adventure Therapy
8th Australian Rural & Remote Mental Health Symposium
www.anzmh.asn.au/rrmh](https://image.slidesharecdn.com/ruralpresentation-161122031310/85/Client-Directed-Recovery-Oriented-Practice-Feedback-Informed-Treatment-to-Improve-Consumer-Participation-15-320.jpg)