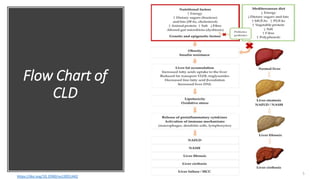
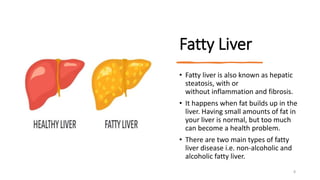
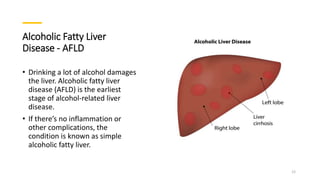
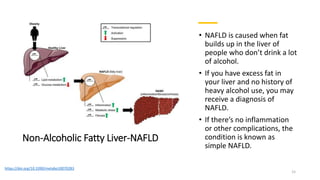
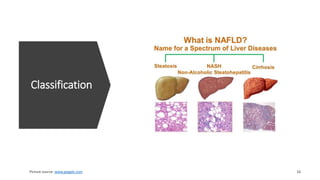
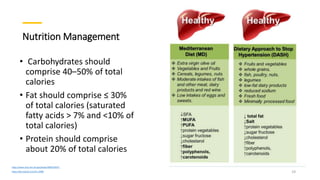
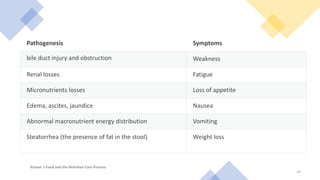
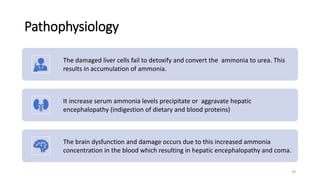
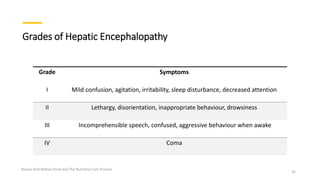
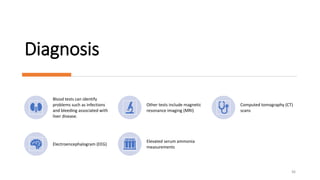
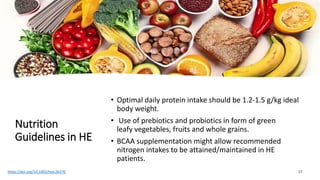
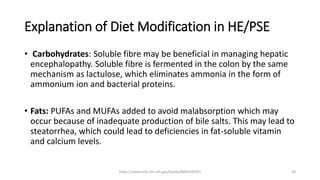
Chronic liver diseases refer to progressive destruction and regeneration of the liver leading to cirrhosis and fibrosis. The main causes include chronic hepatitis B and C, alcoholic fatty liver disease, non-alcoholic fatty liver disease, and others. Symptoms include fatigue, nausea, ascites, and hepatic encephalopathy. Investigation includes blood tests of liver function and imaging. Treatment focuses on managing the underlying cause and complications through diet and lifestyle modifications. Cirrhosis and hepatic encephalopathy are severe complications where scar tissue replaces healthy liver tissue and toxins affect brain function respectively.