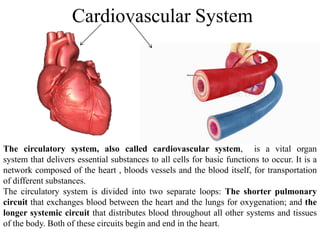
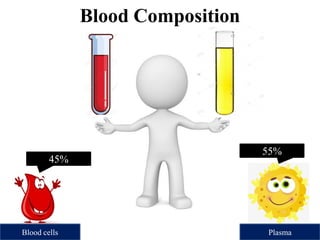
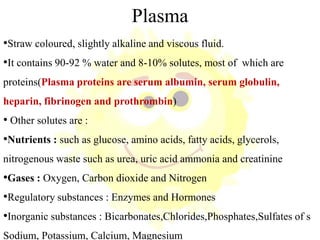
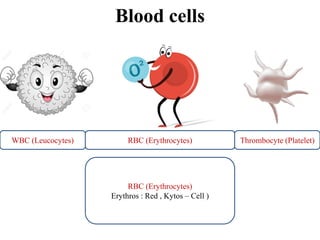
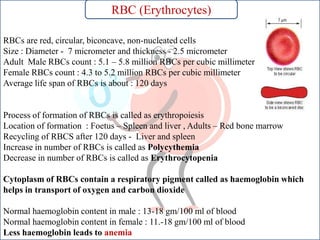
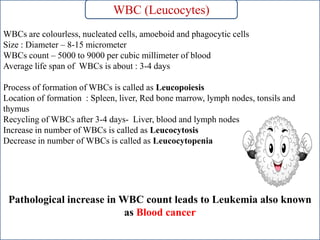
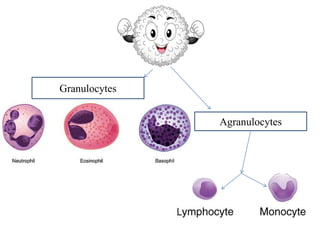
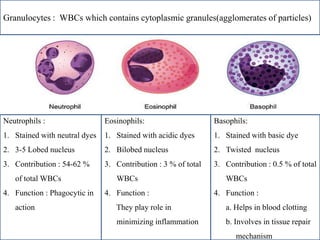
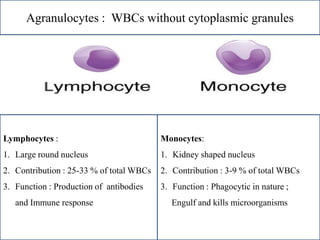
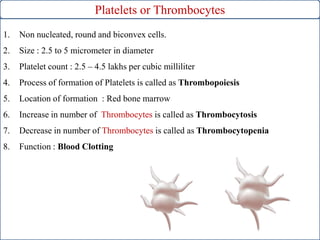
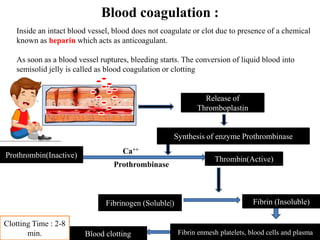
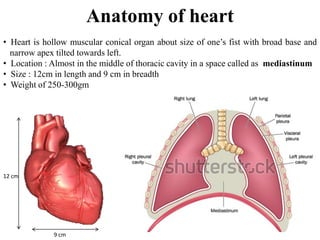
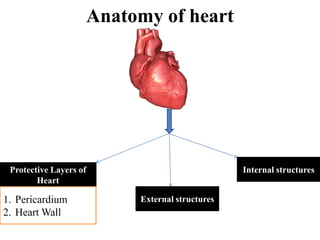
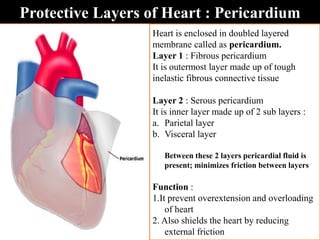
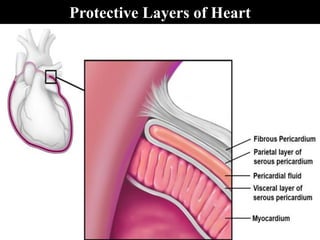
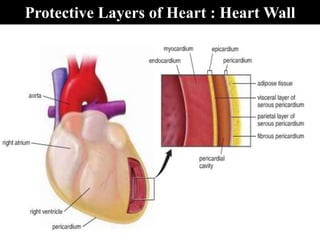
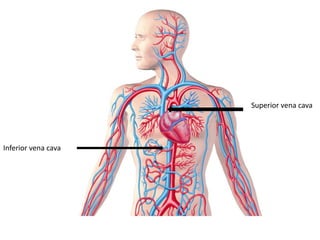
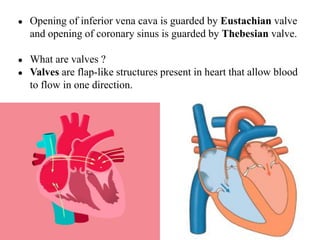
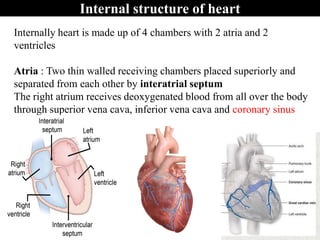
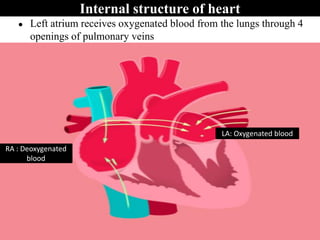
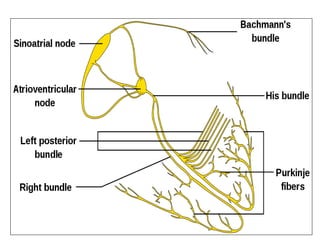
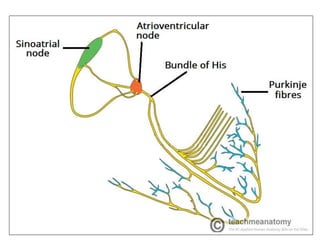
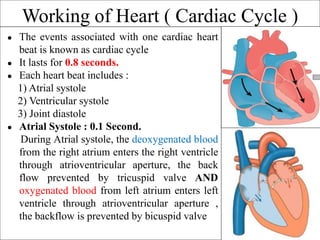
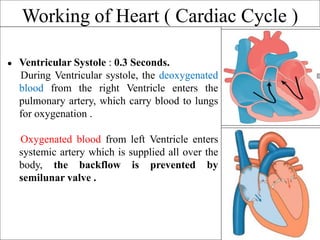
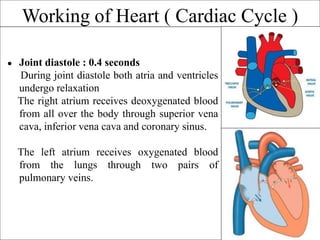
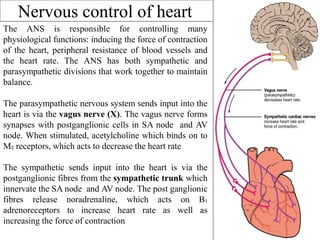
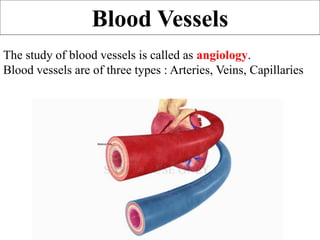
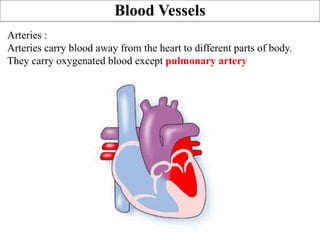
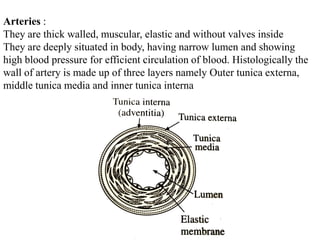
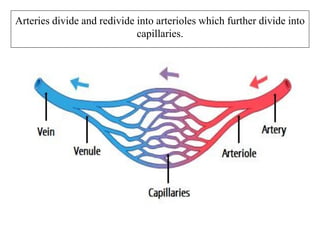
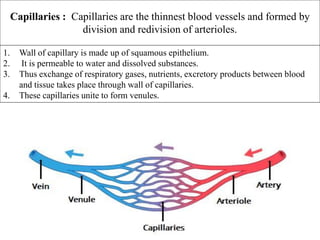
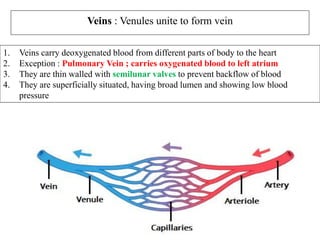
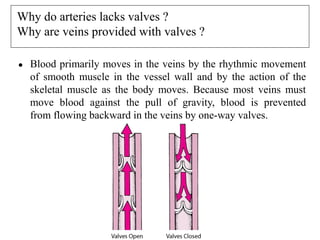
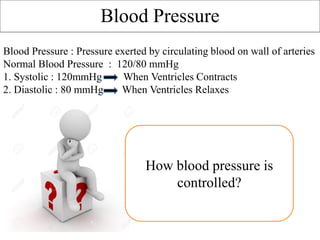
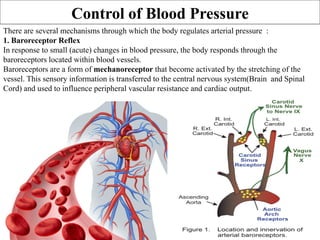
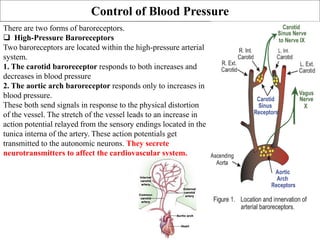
The document provides an in-depth overview of the cardiovascular system, detailing the anatomy and functions of the heart, blood, and blood vessels. It discusses the discovery of blood circulation, the composition and characteristics of blood, and the formation of blood cells. Additionally, it covers mechanisms of blood clotting, cardiac cycle, and regulation of heart rate, emphasizing the roles of both the autonomic nervous system and structural features of the heart and blood vessels.