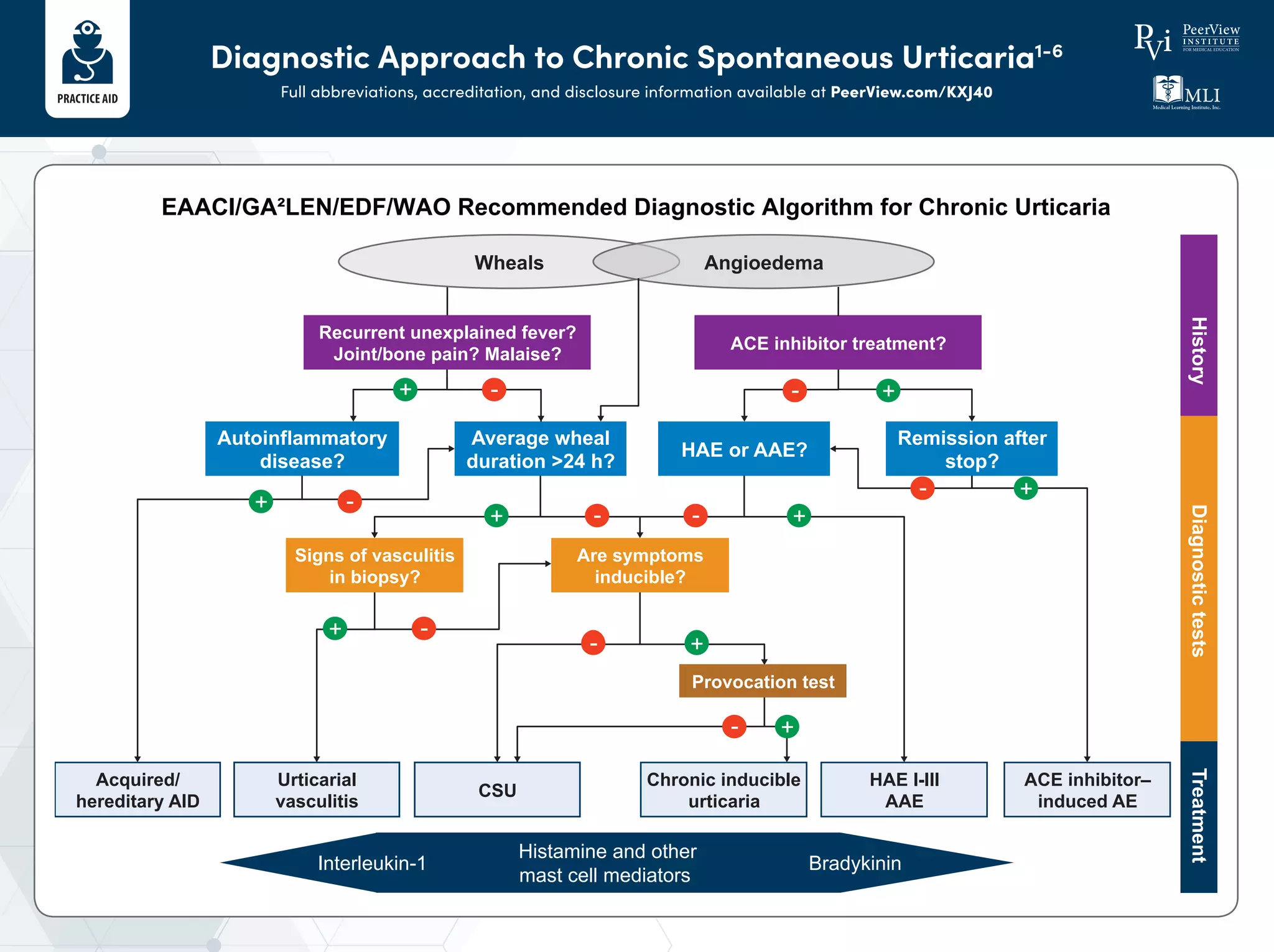
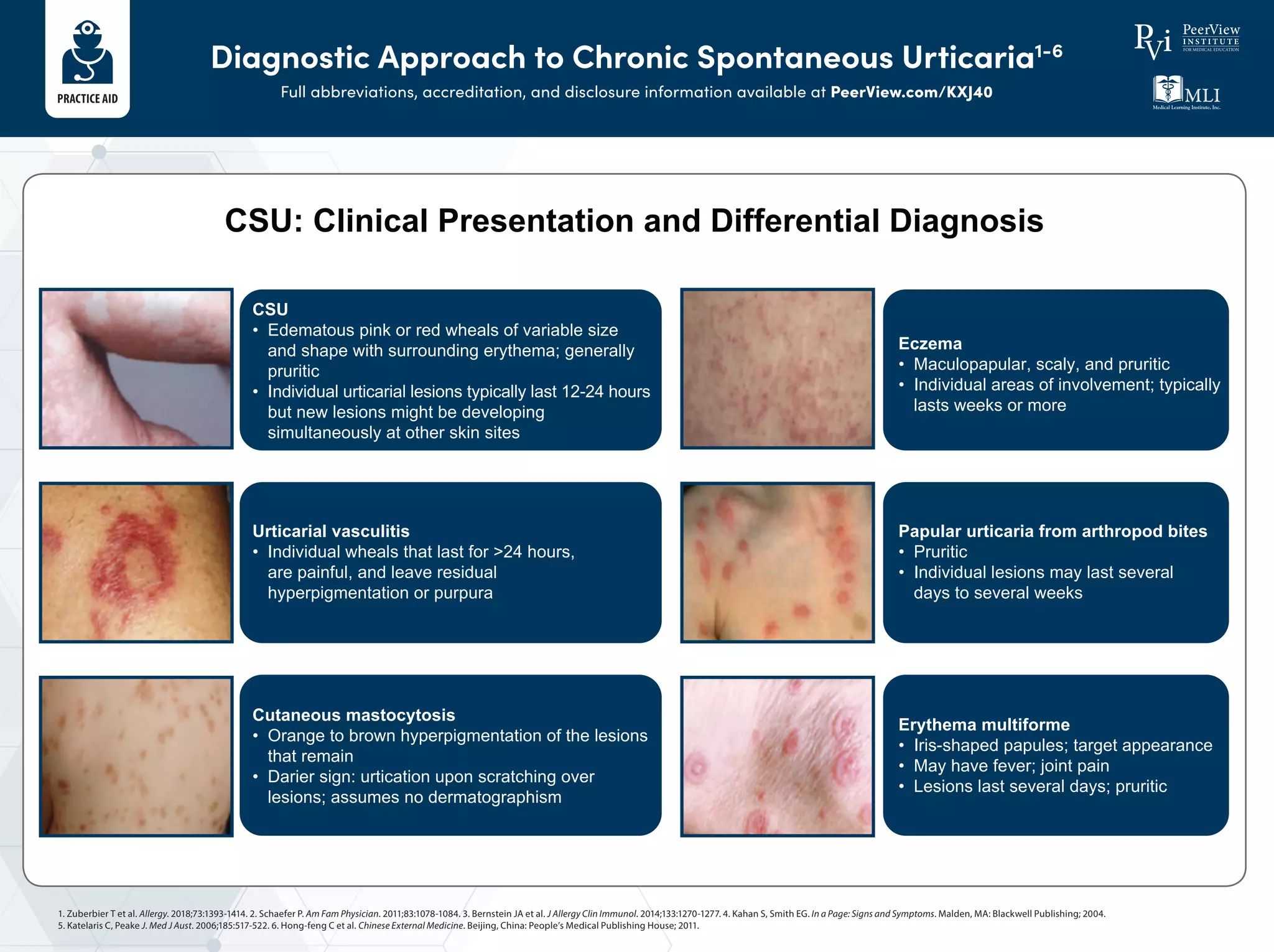
The document outlines a diagnostic and treatment approach for chronic spontaneous urticaria (CSU), detailing various symptoms and differential diagnoses. It presents a stepwise treatment algorithm including different medication options such as antihistamines, omalizumab, and cyclosporine A, depending on the severity of the condition. Additionally, it encourages patients to track their symptoms for better management and to assess treatment response.