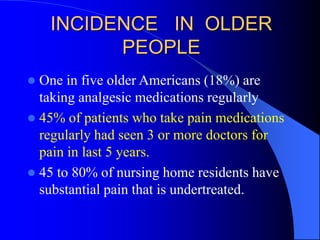
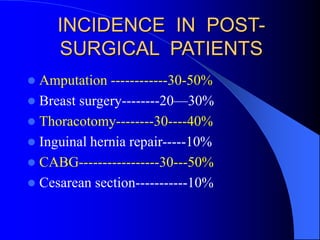
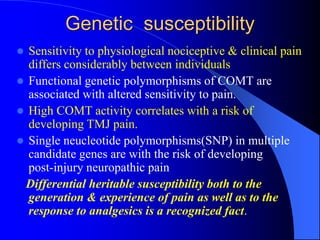
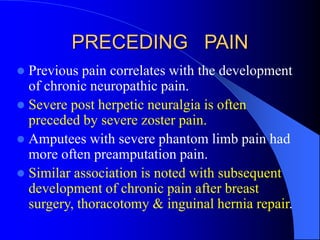
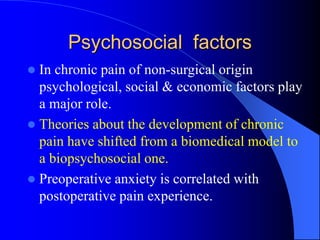
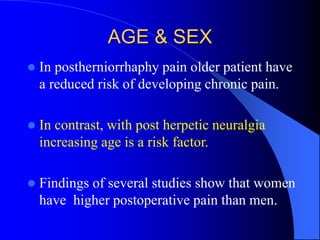
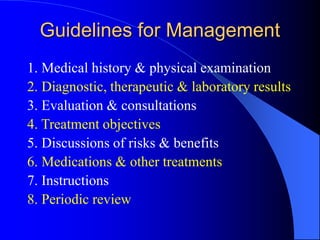
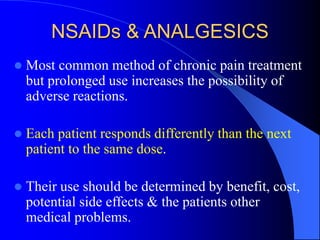
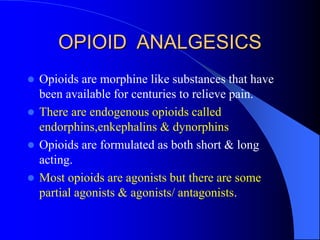
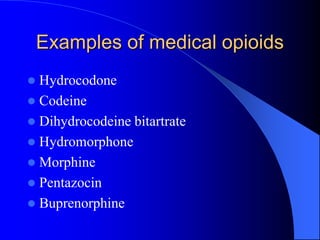
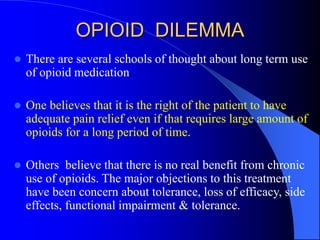
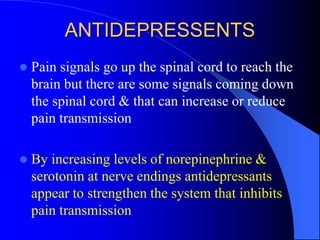
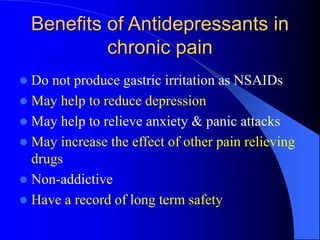
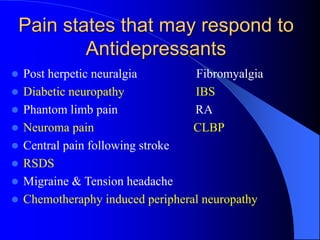
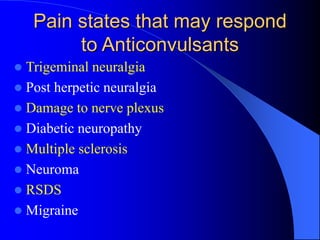
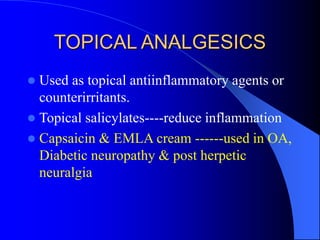
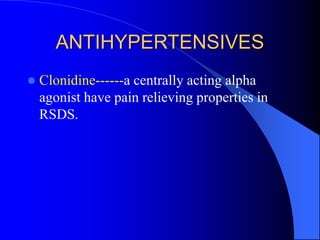
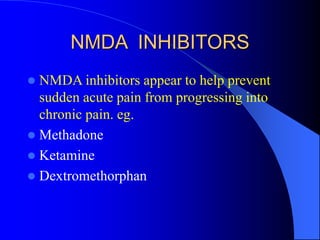
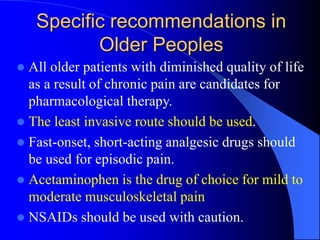
This document discusses chronic pain management in older people. It defines chronic pain as lasting more than 3-6 months and negatively impacting well-being. Chronic pain is classified as nociceptive, inflammatory, neuropathic, or mixed. Risk factors include genetic susceptibility, preceding pain, psychosocial factors, age, and sex. Treatment involves pharmacological options like NSAIDs, opioids, antidepressants, anticonvulsants, and non-pharmacological options like education, exercise, and cognitive behavioral therapy. Specific recommendations are provided for chronic pain management in older adults.