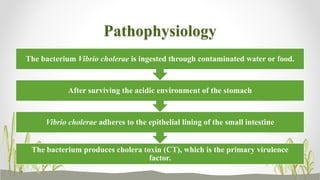
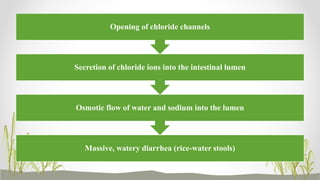
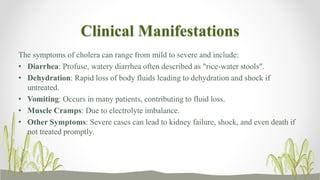
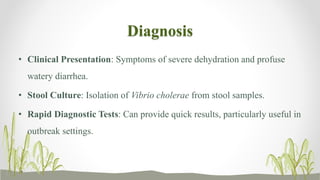
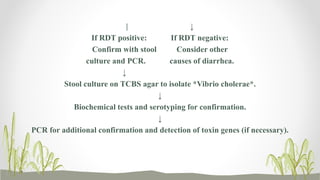
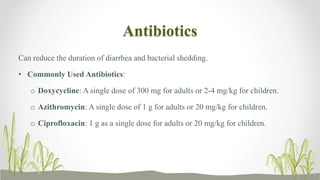
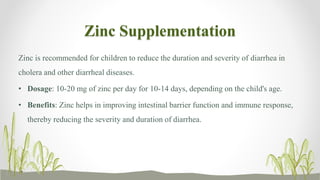
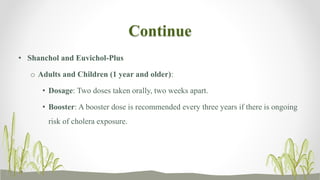
Cholera is an acute diarrheal illness caused by the bacterium Vibrio cholerae, primarily transmitted through contaminated water and food. Symptoms range from mild to severe, including profuse watery diarrhea and dehydration, with diagnosis based on clinical presentation and stool culture. Treatment focuses on rehydration, antibiotics, and zinc supplementation, while prevention strategies involve improving water sanitation, hygiene practices, and vaccination for at-risk populations.