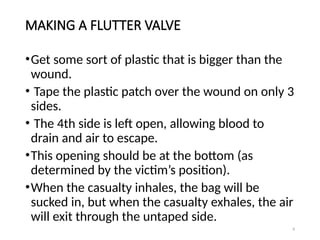
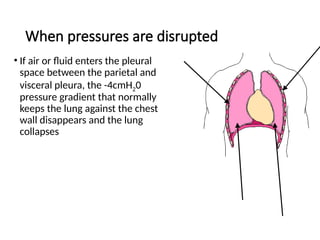
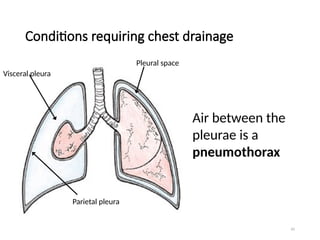
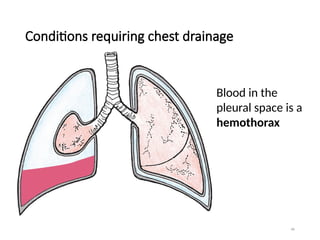
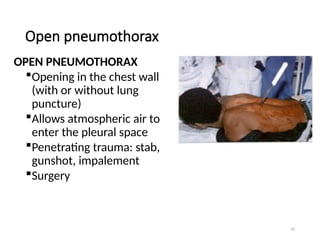
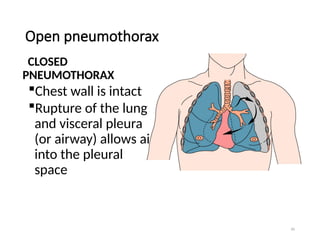
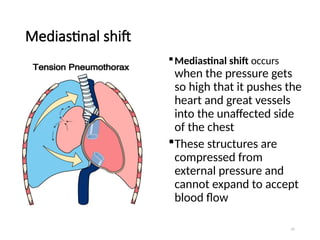
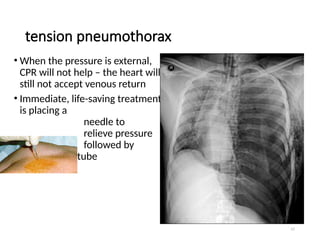
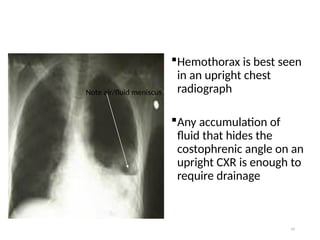
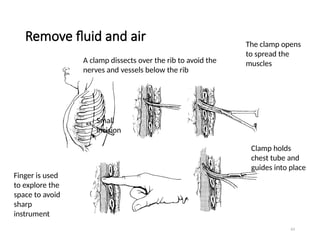
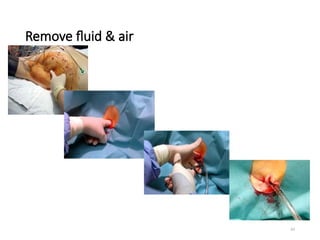
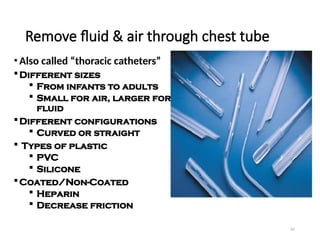
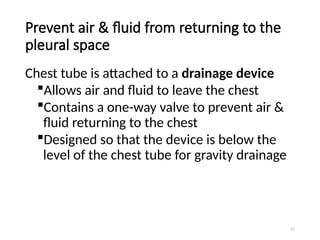
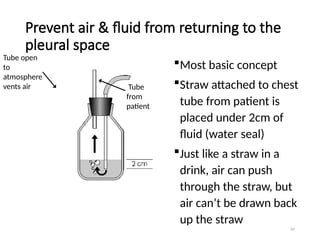
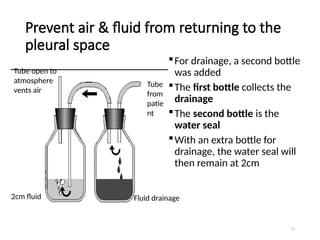
The document discusses various types of chest injuries, including closed and open chest wounds, pneumothorax, hemothorax, and their treatments. It highlights the importance of recognizing and managing these injuries to prevent serious complications and emphasizes on assessment and monitoring of the patient's condition. Additionally, it covers surgical interventions like thoracostomy and thoracotomy, along with management strategies for specific conditions such as lung contusions and empyema.