This document discusses various topics relating to workforce safety and wellness for EMTs, including:
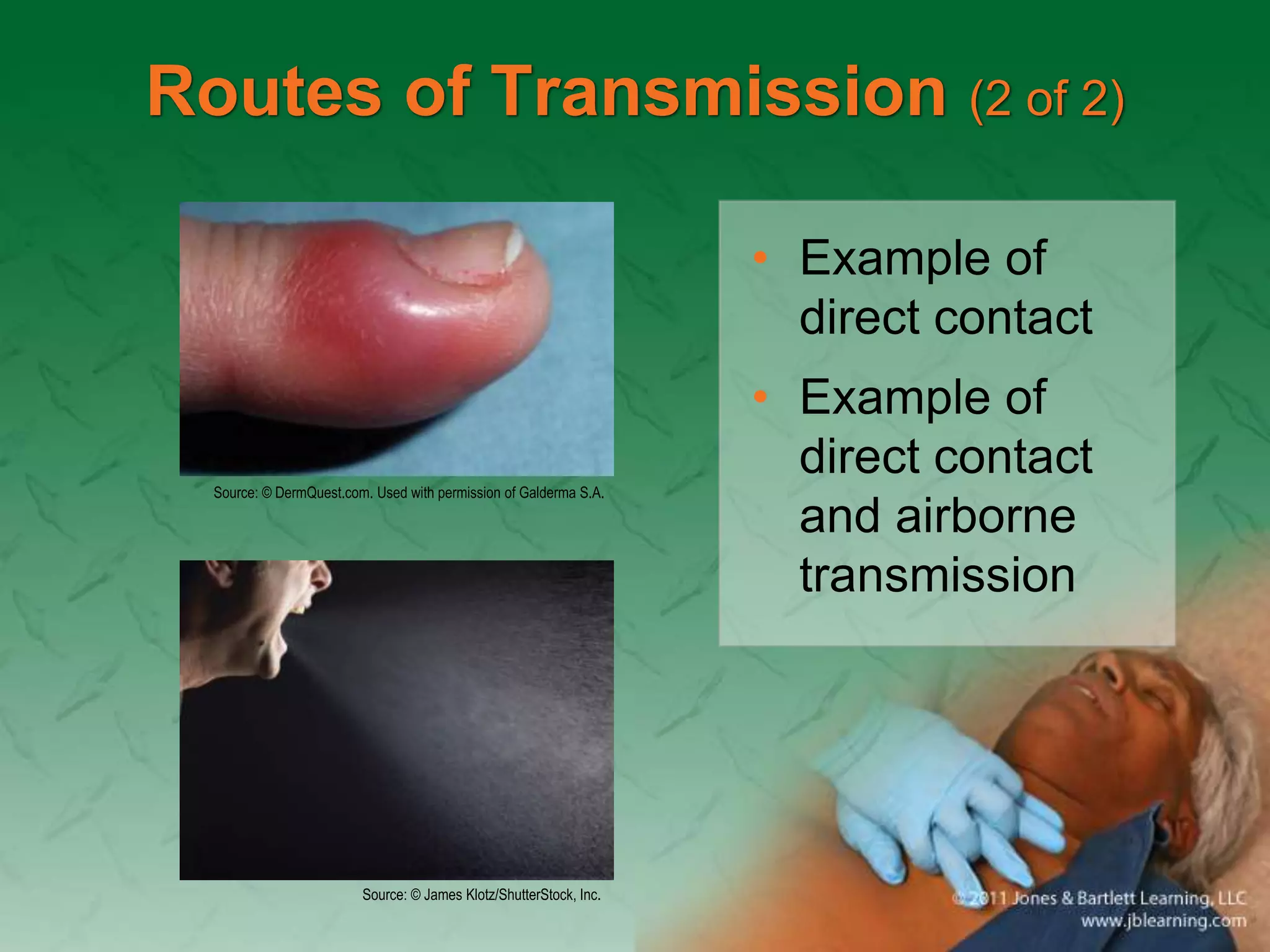
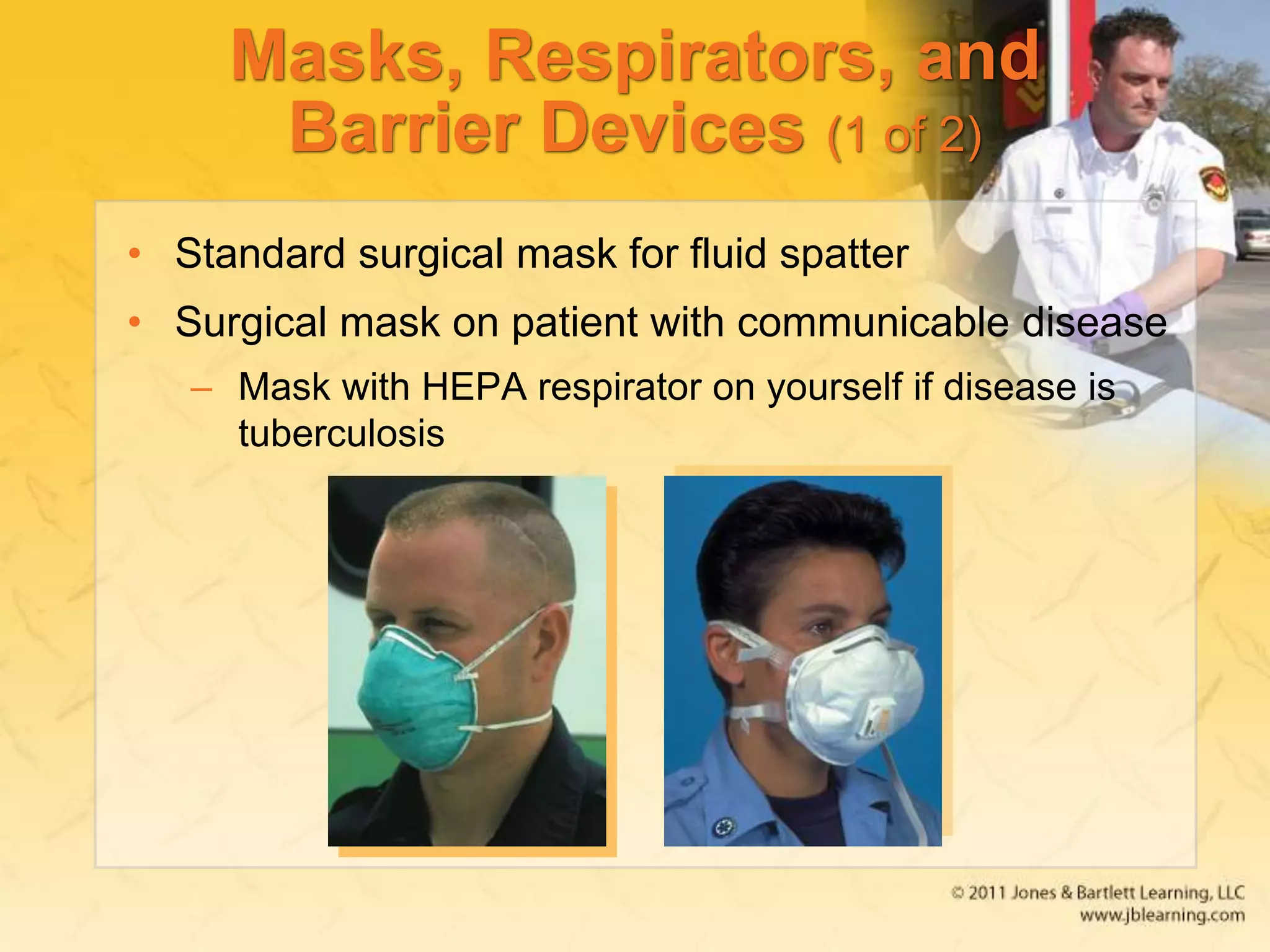
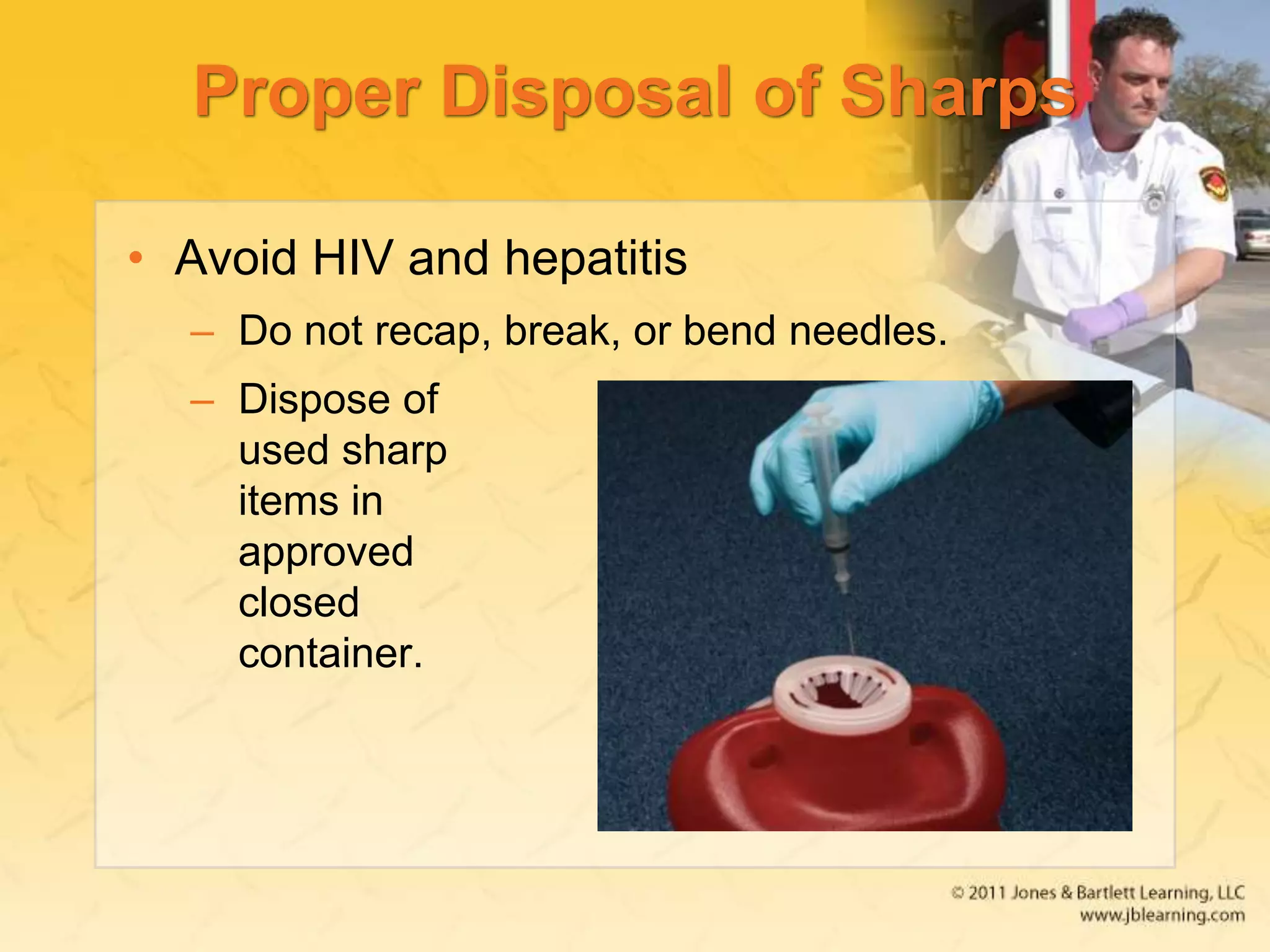
1) Infectious diseases can spread between people and minimizing risk through immunizations, handwashing, and protective equipment.
2) EMTs face stress and hazards on the job which can be managed through self-care, social support, and developing stress management routines.
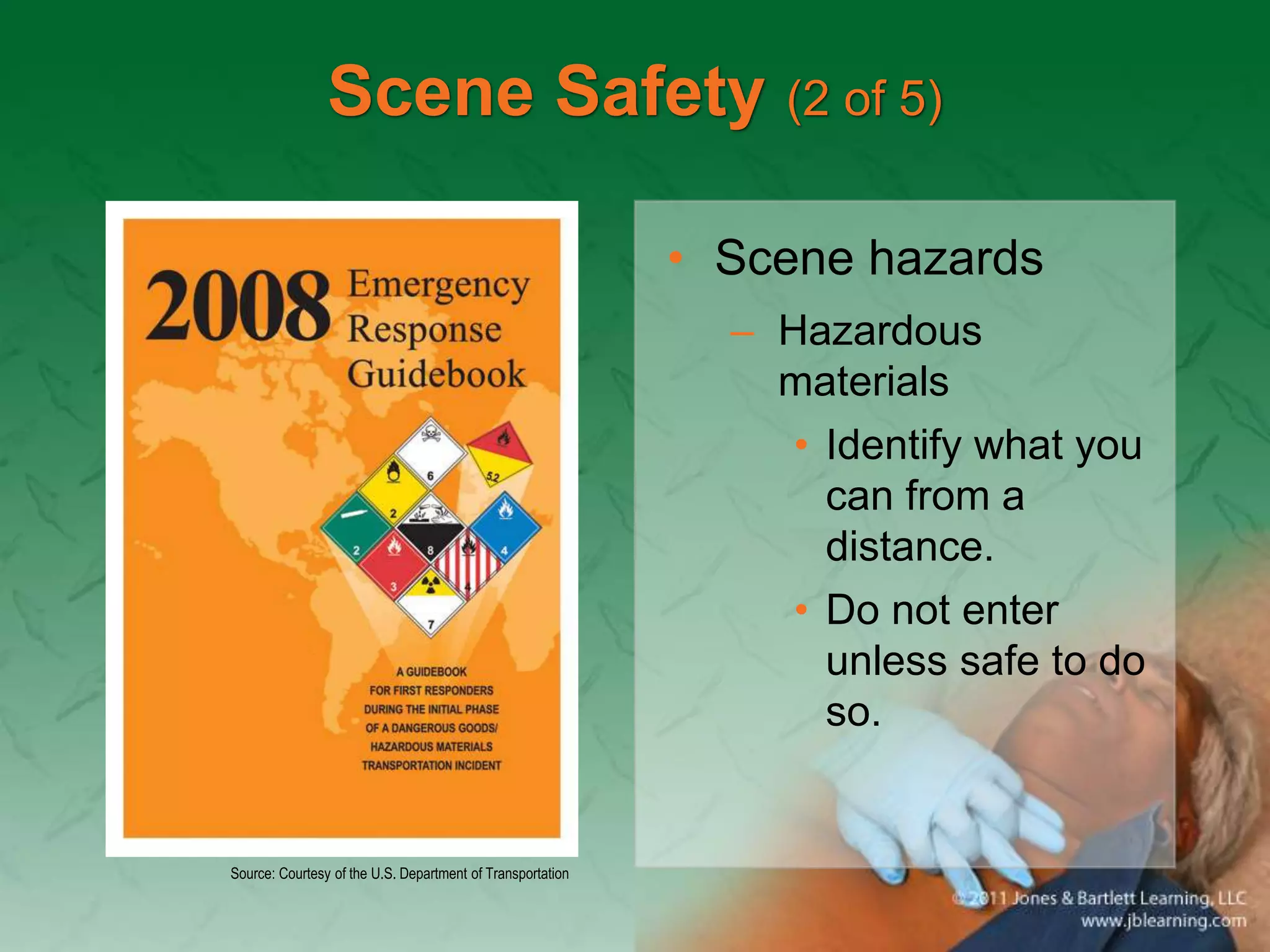
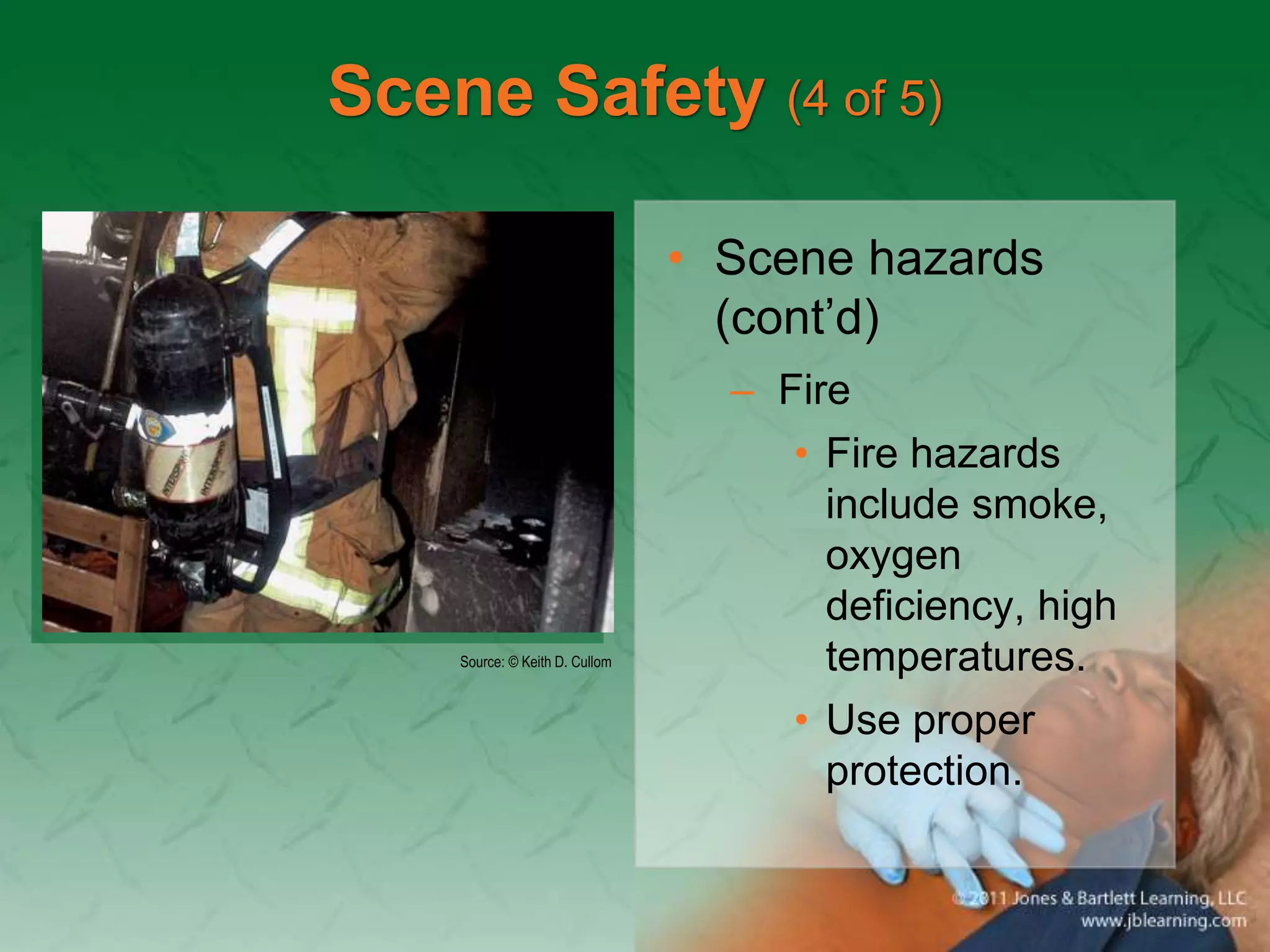
3) Proper safety protocols and protective equipment are necessary for ensuring EMTs avoid exposure to infectious diseases, violence, and other hazards when responding to emergency calls.