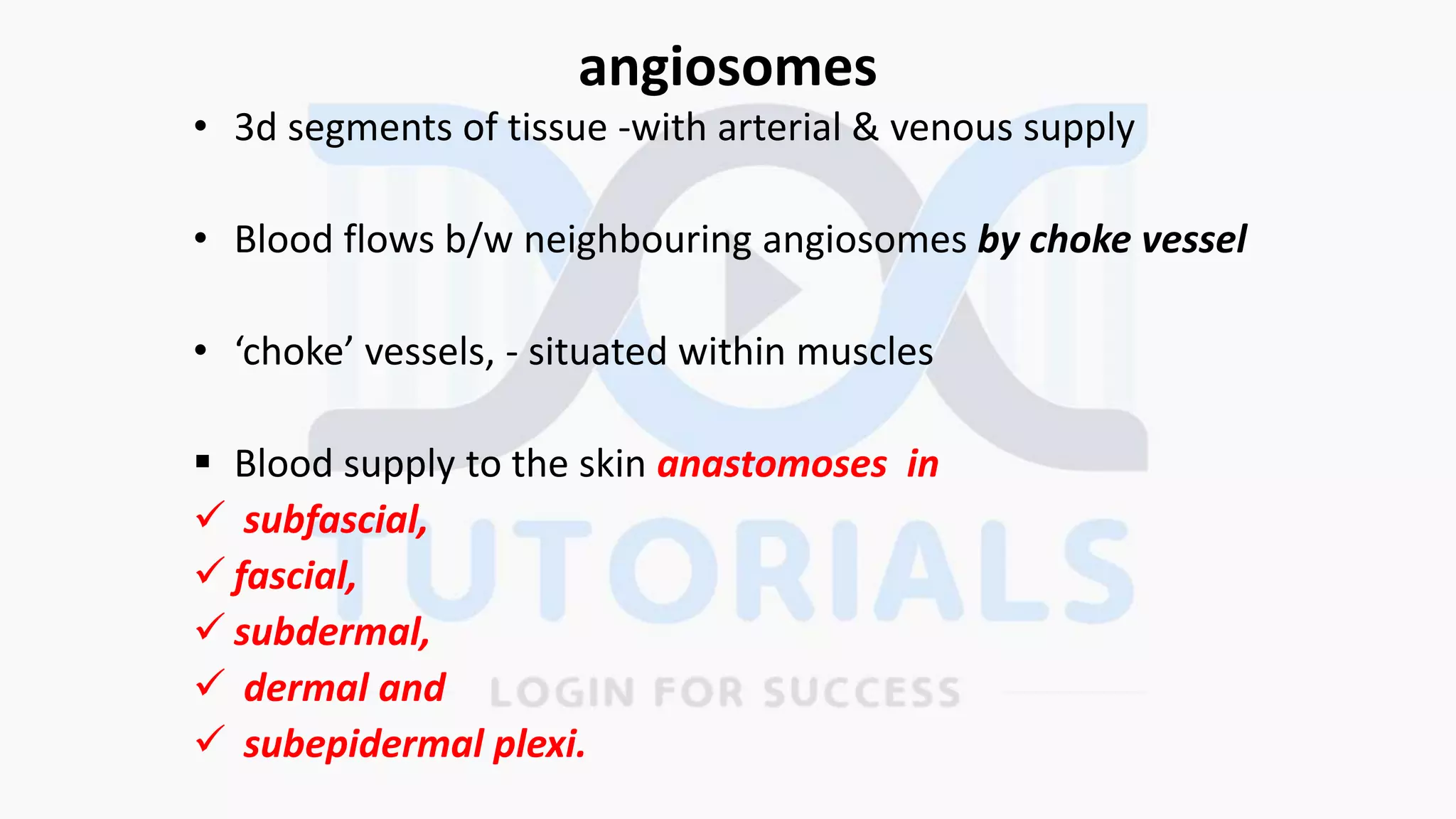
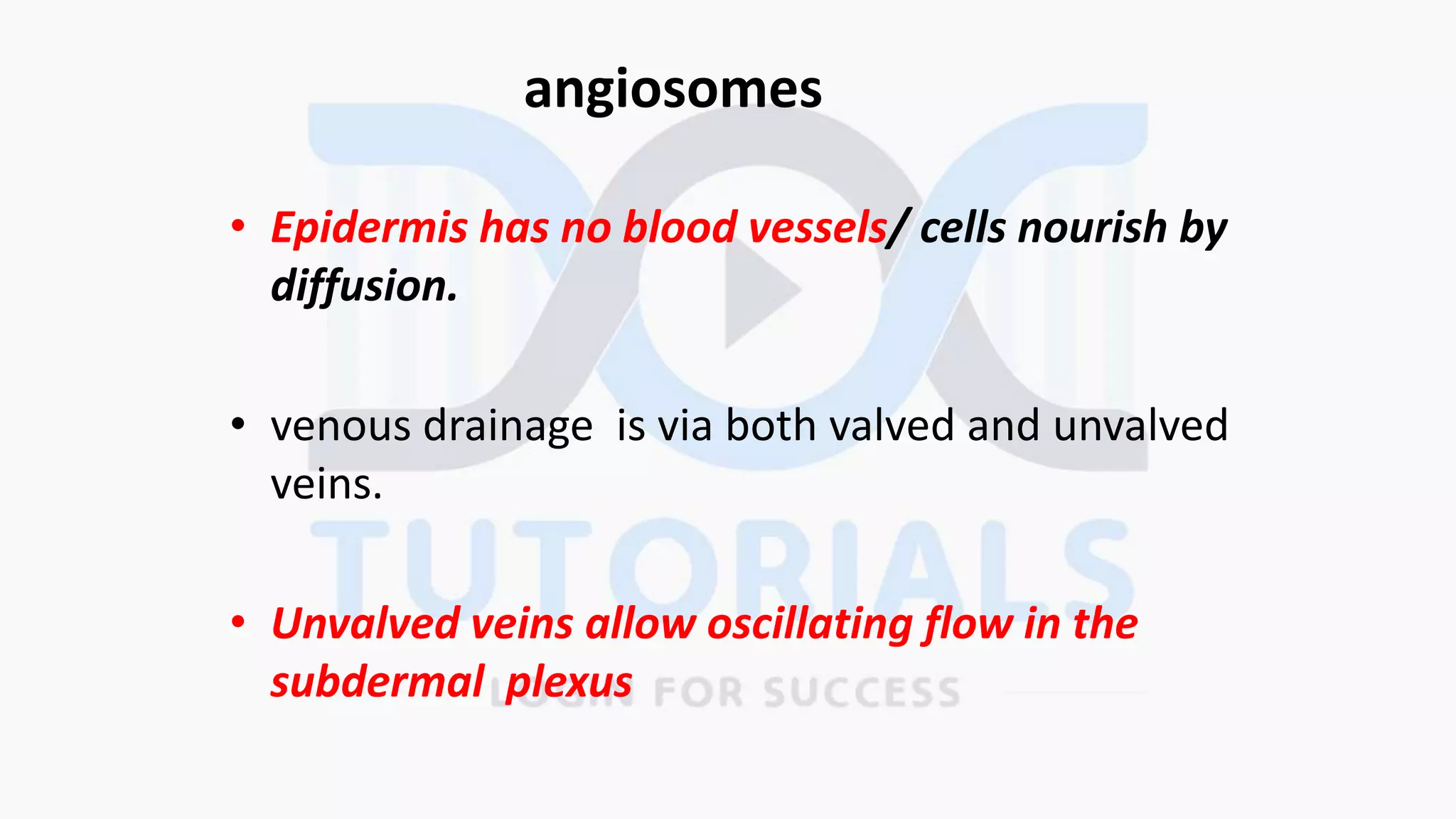
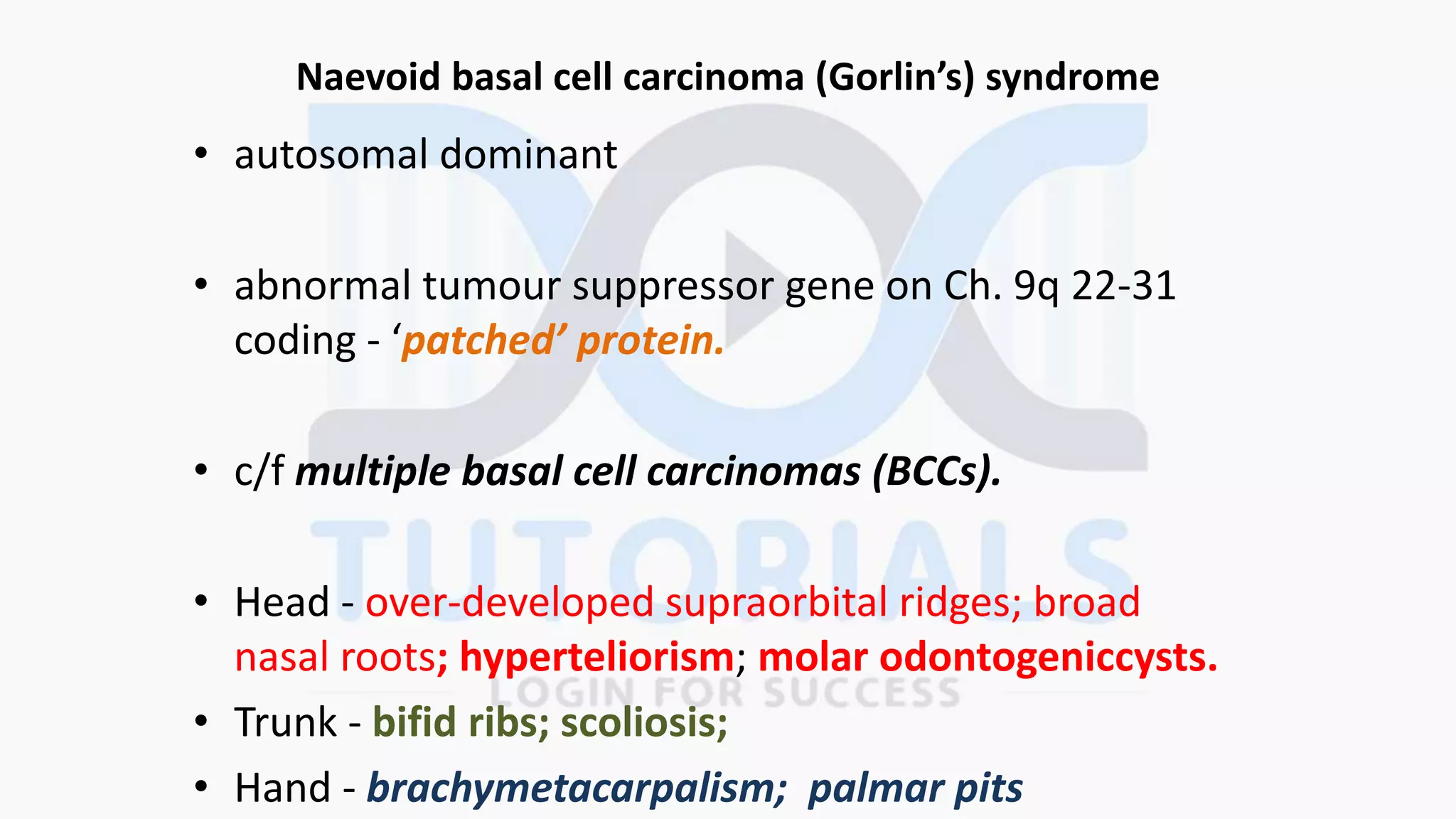
This document summarizes key aspects of skin and subcutaneous tissues. The epidermis is the outermost layer of skin, consisting of stratified squamous epithelium. Keratinocytes grow and are replaced by mitosis in the stratum granulosum. Melanocytes are dendritic cells located in the basal epidermis that transfer melanin to keratinocytes via membrane processes. There are two main types of sweat glands - eccrine glands which secrete sweat throughout the body, and apocrine glands which secrete in response to emotions and hormones in the axillae and groins. The document also discusses various skin tumors, lesions, and conditions.