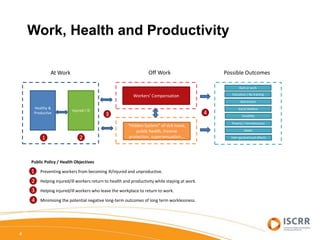
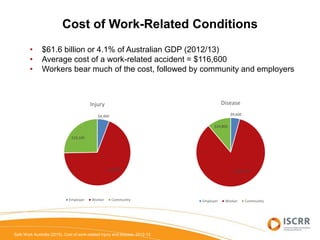
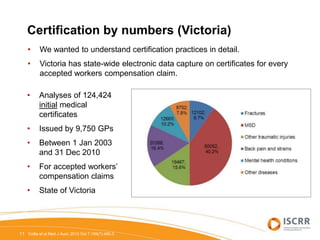
The document discusses the link between work, health, and productivity, highlighting the high incidence of work-related injuries in Australia and their economic impacts. It emphasizes the role of general practitioners (GPs) in issuing sickness certificates, which are crucial for worker compensation and return-to-work processes, while identifying barriers faced by GPs, including administrative burdens and communication issues. Despite the introduction of initiatives like the 'fit note' aimed at improving return-to-work outcomes, the effectiveness of these changes remains uncertain, stressing the need for ongoing efforts to enhance certification practices.















![“They [insurance case managers] keep changing. And I have to ask,
‘Well why do these workers keep changing?’ Why is one patient who
is in the system for a long time, constantly handed on to another
worker who doesn’t know the patient, doesn't know their background?
I might have 15 years of knowledge of the patient ... I feel like we have
continuity of care and the system doesn’t”
(GP25, m, 50yo, 25ye).
20
Compensation system barriers
Brijnath B et alJ Occup Rehabil. 2014 Dec;24(4):766-76](https://image.slidesharecdn.com/collienthqldrtwconferenceapril2016finalpublic-160504003333/85/Certifying-Capacity-for-Work-20-320.jpg)