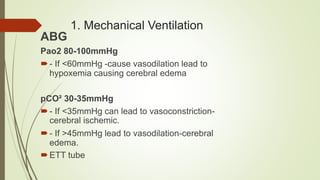
This document provides information on cerebral protection for nurses. It defines cerebral protection as interventions to improve neurological outcomes for patients at risk of cerebral ischemia and prevent secondary brain injury. It lists 14 interventions for cerebral protection, including maintaining adequate oxygenation and ventilation, managing hemodynamics, monitoring intracranial pressure, maintaining normothermia, providing DVT prophylaxis, and maintaining electrolyte balance. The goal of these interventions is to prevent further cerebral damage, reverse existing damage, and improve cerebral functions and neurological outcomes.