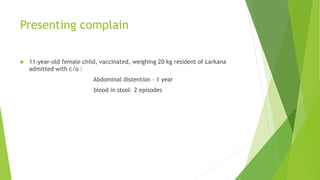
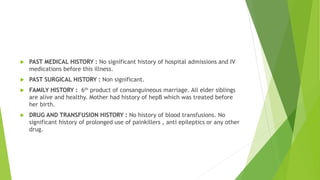
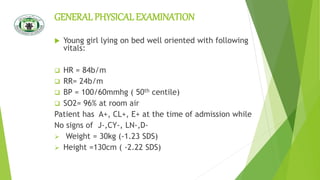
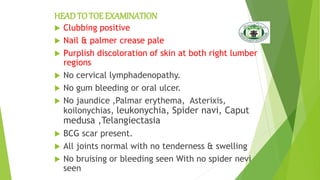
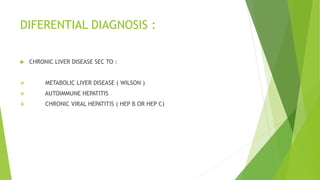
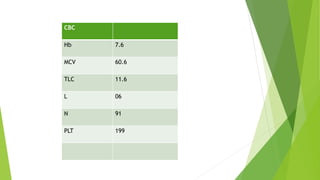
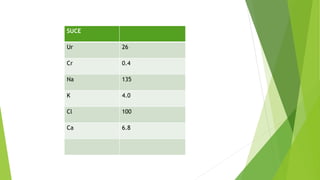
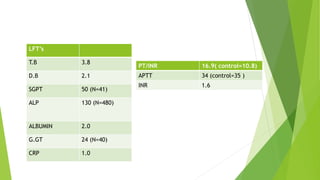
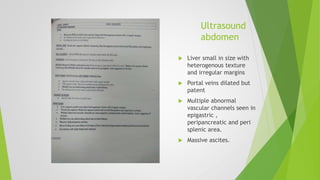
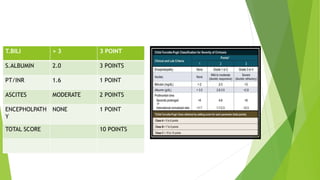
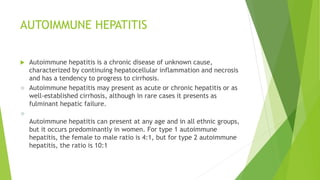
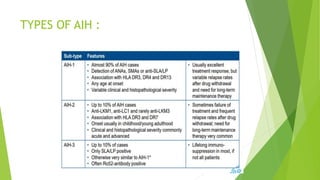
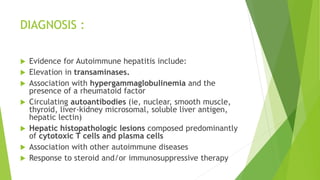
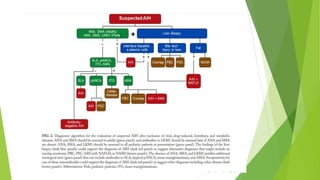
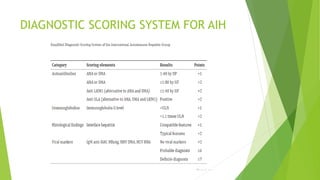
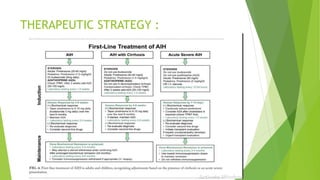
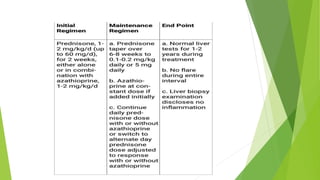
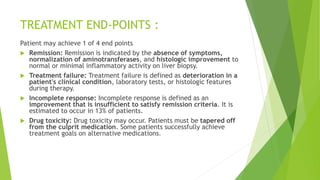
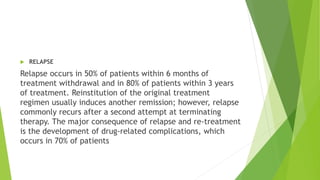
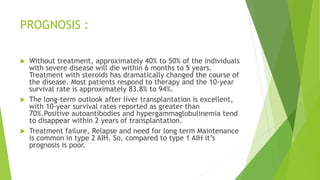
This document describes a case of an 11-year-old female child presenting with abdominal distension and blood in stool. Various tests were performed and findings were consistent with cirrhosis of the liver with portal hypertension. Further workup revealed positive ANA and ASMA antibodies, consistent with a diagnosis of autoimmune hepatitis. Autoimmune hepatitis is a chronic disease of unknown cause characterized by liver inflammation and necrosis that can progress to cirrhosis. It has two main types and is diagnosed based on elevated enzymes, antibodies, and histopathology. Treatment involves immunosuppression with steroids and medications, with the goal of achieving remission though relapse is common.