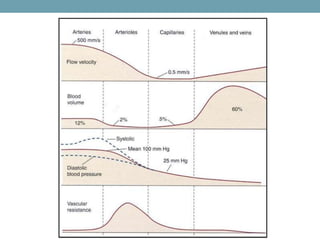
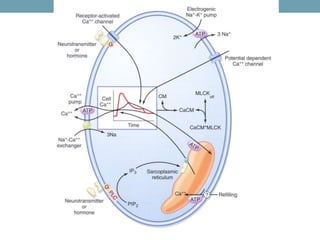
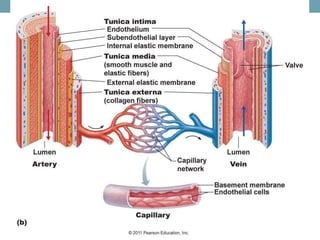
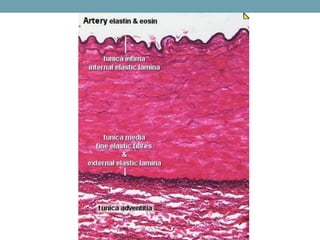
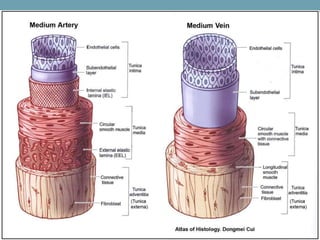
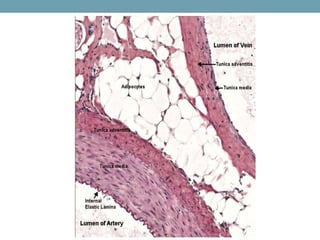
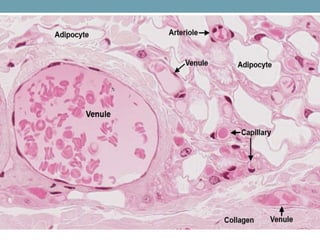
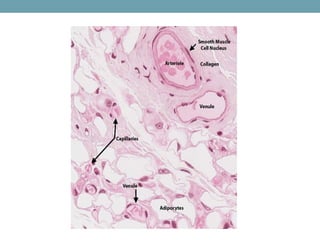
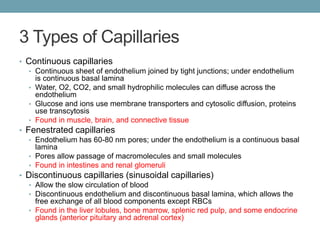
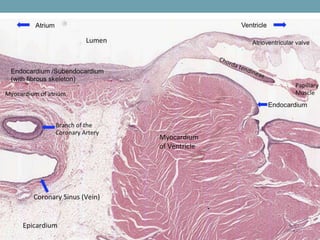
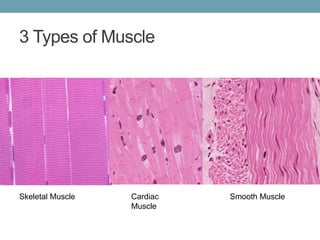
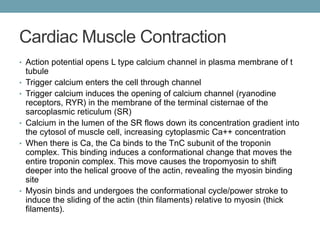
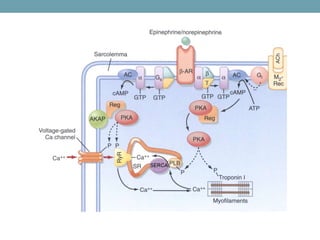
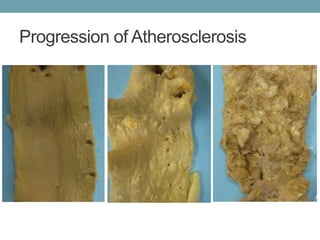
This document summarizes the structure and function of blood vessels and heart tissue. It describes the different types of blood vessels including arteries, veins, and capillaries. It discusses the layers of blood vessels and the cells that make up each layer. The document also summarizes the structure and function of cardiac muscle and compares the three main types of muscle tissue. Finally, it provides an overview of atherosclerosis and several heart conditions.