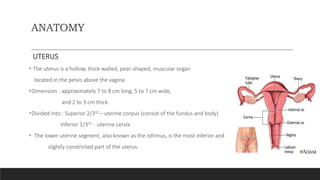
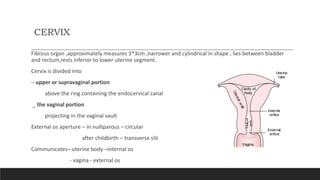
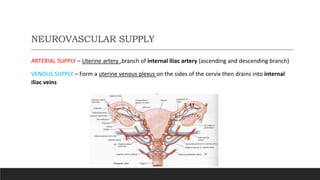
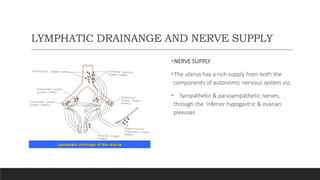
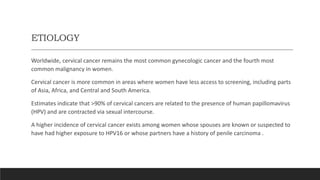
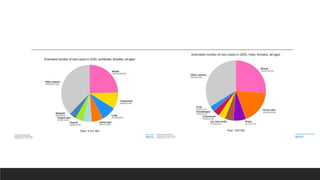
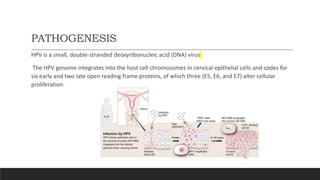
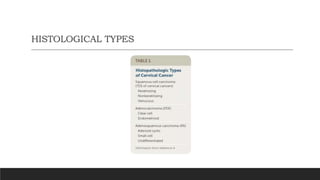
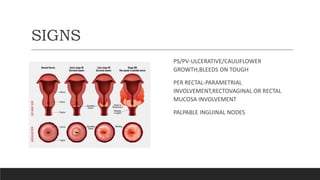
The document provides a comprehensive overview of cervical cancer, including the anatomy of the uterus and cervix, its etiology linked predominantly to human papillomavirus (HPV) infection, and various risk factors associated with the disease. It details the pathogenesis, symptoms, histological types, methods for investigation, and treatment options, which range from surgery to chemotherapy and radiotherapy. Cervical cancer remains the most common gynecologic cancer globally, particularly in regions with limited screening access.