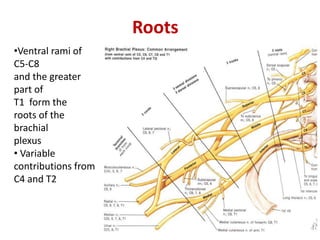
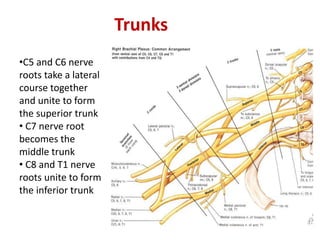
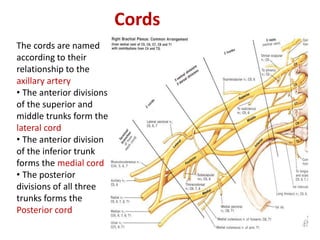
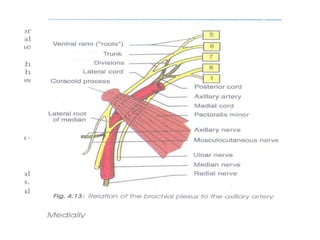
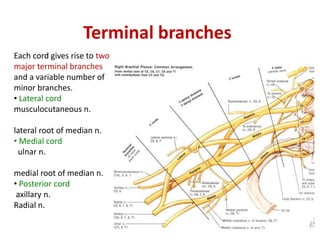
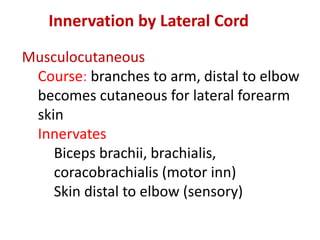
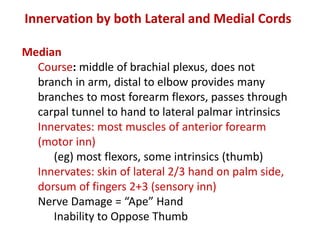
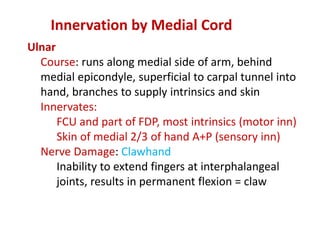
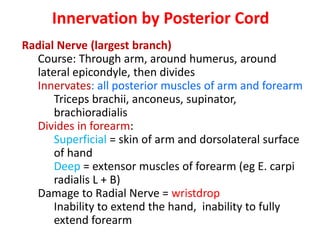
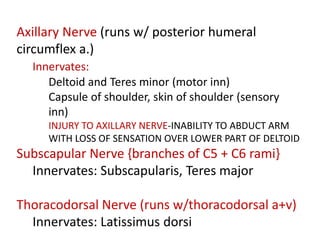
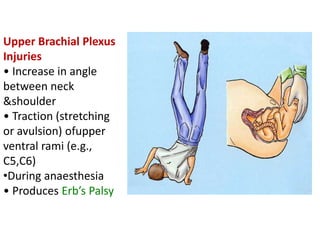
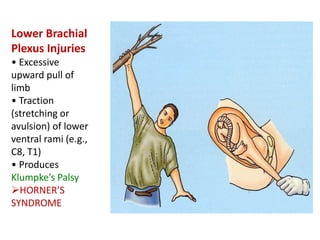
The brachial plexus is formed from the ventral rami of cervical and upper thoracic nerve roots. It divides into trunks, divisions, cords, and terminal branches that innervate the upper limb. The superior, middle, and inferior trunks are formed from nerve root contributions. The cords are the lateral, medial, and posterior cords. Each cord gives rise to terminal branches that innervate specific muscles and skin. Injuries can occur at different levels and cause deficits such as winged scapula, claw hand, or wrist drop depending on the affected nerves.