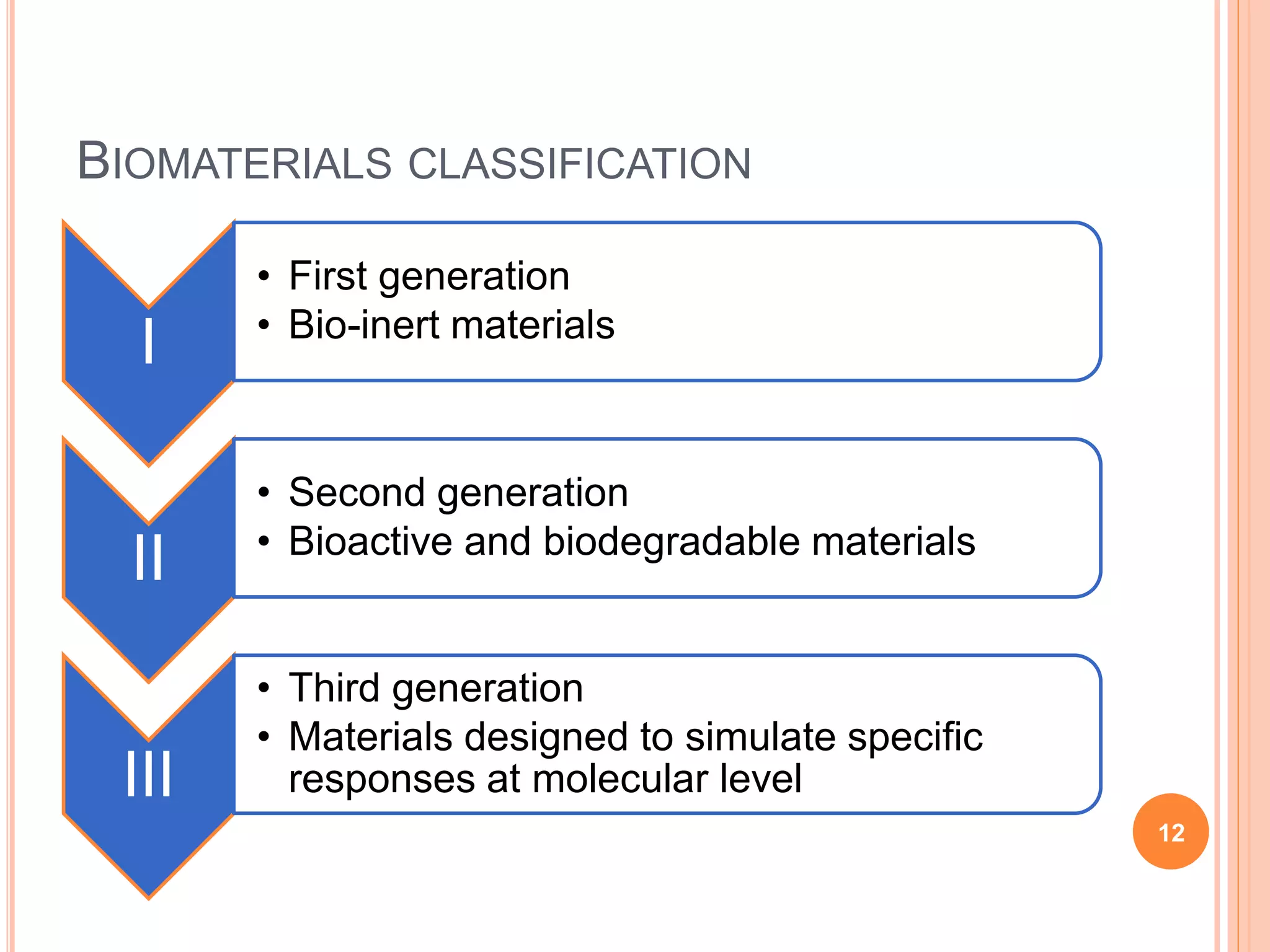
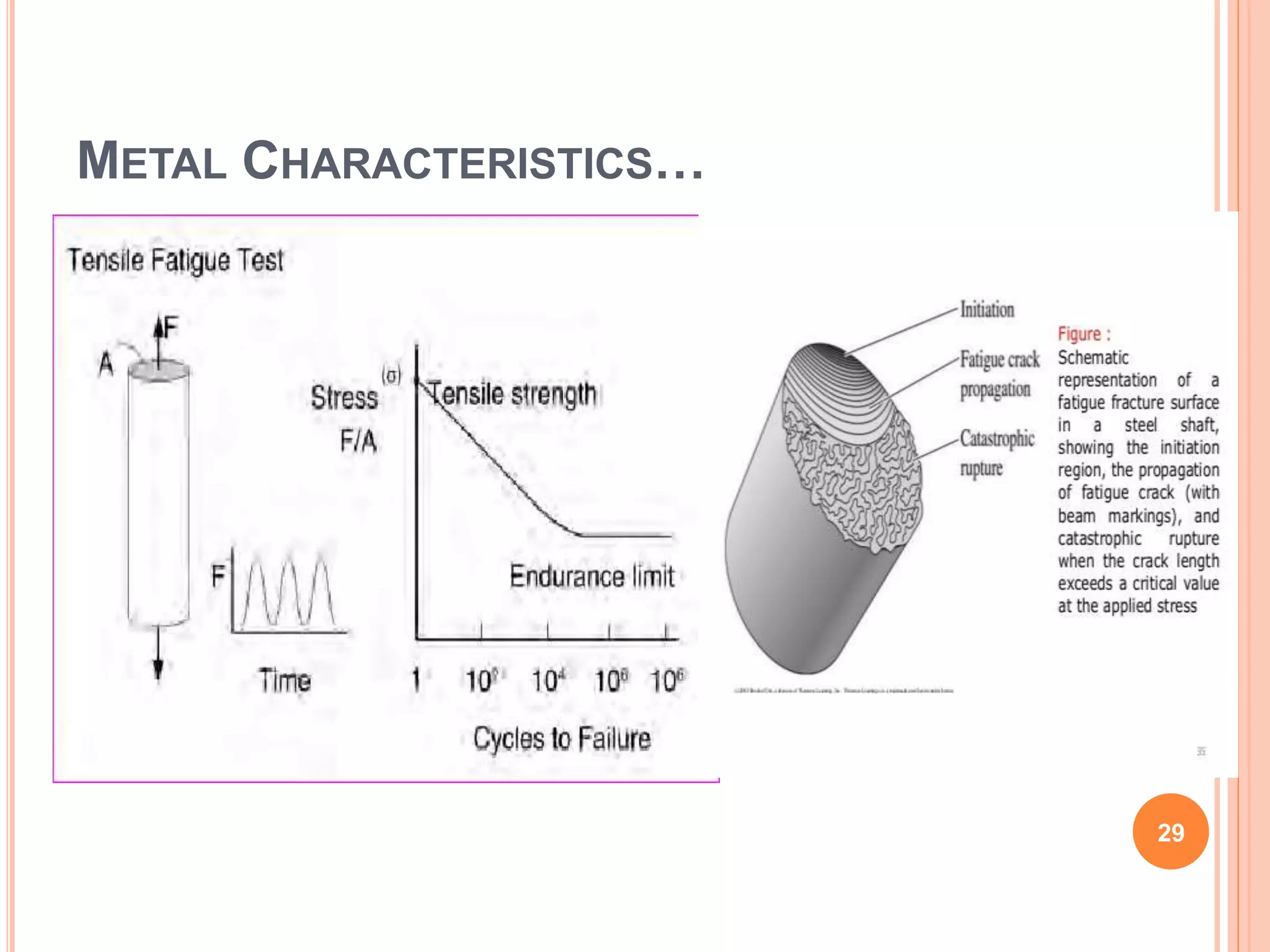
This document provides an overview of biomaterials used in orthopaedics. It begins with objectives of discussing properties of commonly used biomaterials and giving an introduction to basic biomaterial science. The introduction defines biomaterials and discusses their early history and qualities needed for biomedical applications. Commonly used biomaterials are then categorized as metals, polymers, and ceramics. Metallic biomaterials discussed include stainless steel, cobalt-chromium alloys, titanium alloys, and the newer tantalum. Key properties like mechanical behavior, strength, corrosion, and structural characteristics are reviewed for understanding biomaterial selection and performance.










































































![CERAMICS…
Examples:
Inert
Silica (SiO2), Alumina (Al2O3), Zirconia (ZrO2)
Bioactive
Hydroxyapatite [Ca10(PO4)6(OH)2]
Tricalcium phosphate [Ca3(PO4)2]
87](https://image.slidesharecdn.com/biomaterials-210331124246/75/Biomaterials-in-Orthopaedics-87-2048.jpg)





















