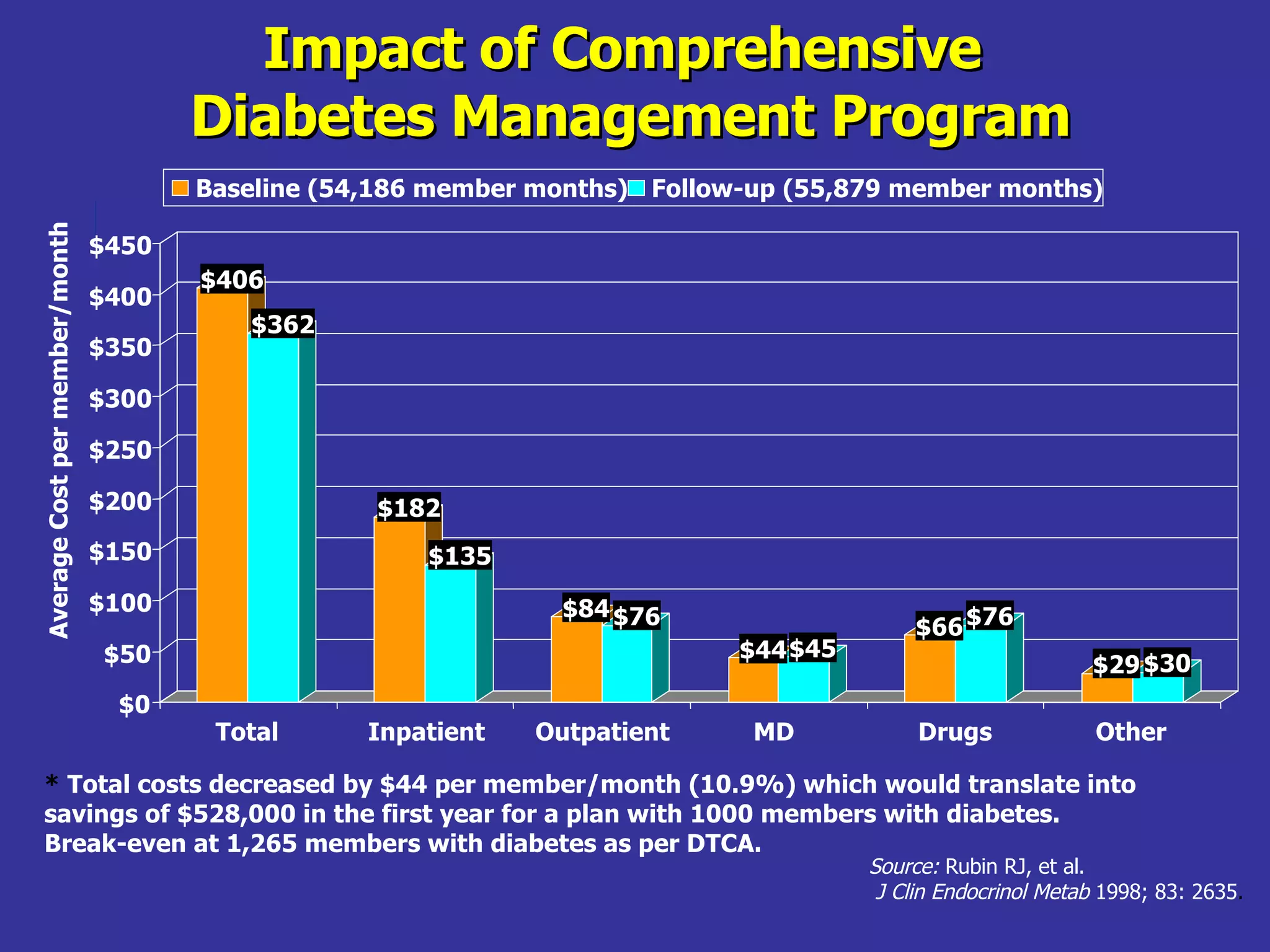
The document discusses components of a diabetes care team including dietitians, endocrinologists, nurses, exercise therapists, and primary care physicians. It also outlines the stages of patient health education, characteristics of health educators, factors affecting the learning process, and ways to evaluate educational programs.