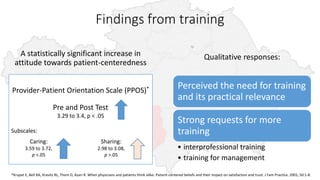
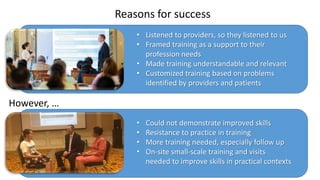
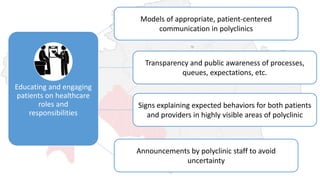
The document discusses the outcomes of communication training aimed at improving patient-centered care among healthcare providers, showing statistically significant increases in attitudes towards patient-centeredness. Key success factors included addressing provider needs, customizing content, and a strong desire for ongoing training, while challenges involved demonstrating improved skills and resistance to training practices. Moving forward, the document emphasizes the need for continued education for both providers and patients, as well as enhanced integration of communication strategies in medical training.