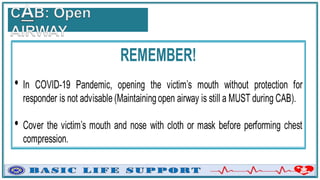
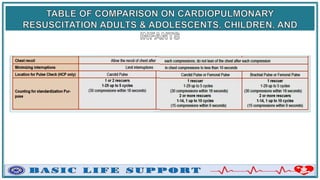
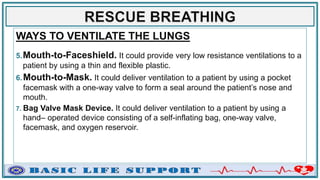
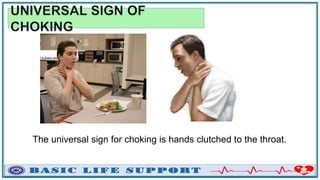
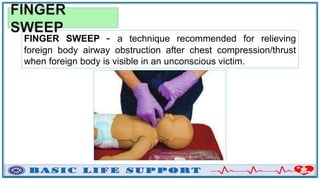
The document provides comprehensive guidelines on emergency care principles, including basic life support (BLS), cardiopulmonary resuscitation (CPR) methods, and emergency action principles. It outlines the steps for assessing and managing cardiac arrest situations, the use of automated external defibrillators (AEDs), and the importance of scene safety and proper logistics. Additionally, it highlights the American Heart Association's chain of survival and offers specific techniques for CPR on adults, children, and infants, along with relevant protocols for airway obstruction management.