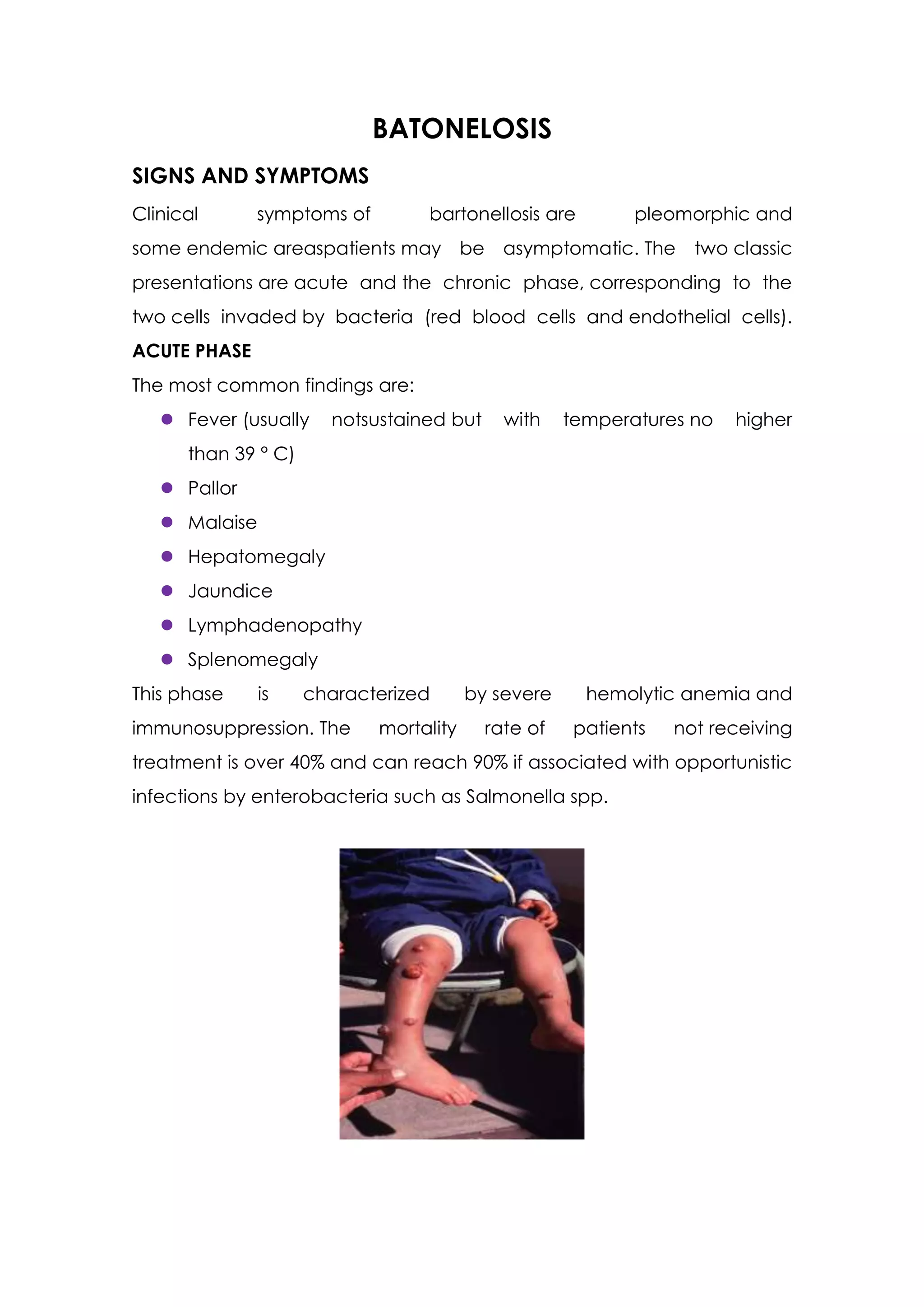
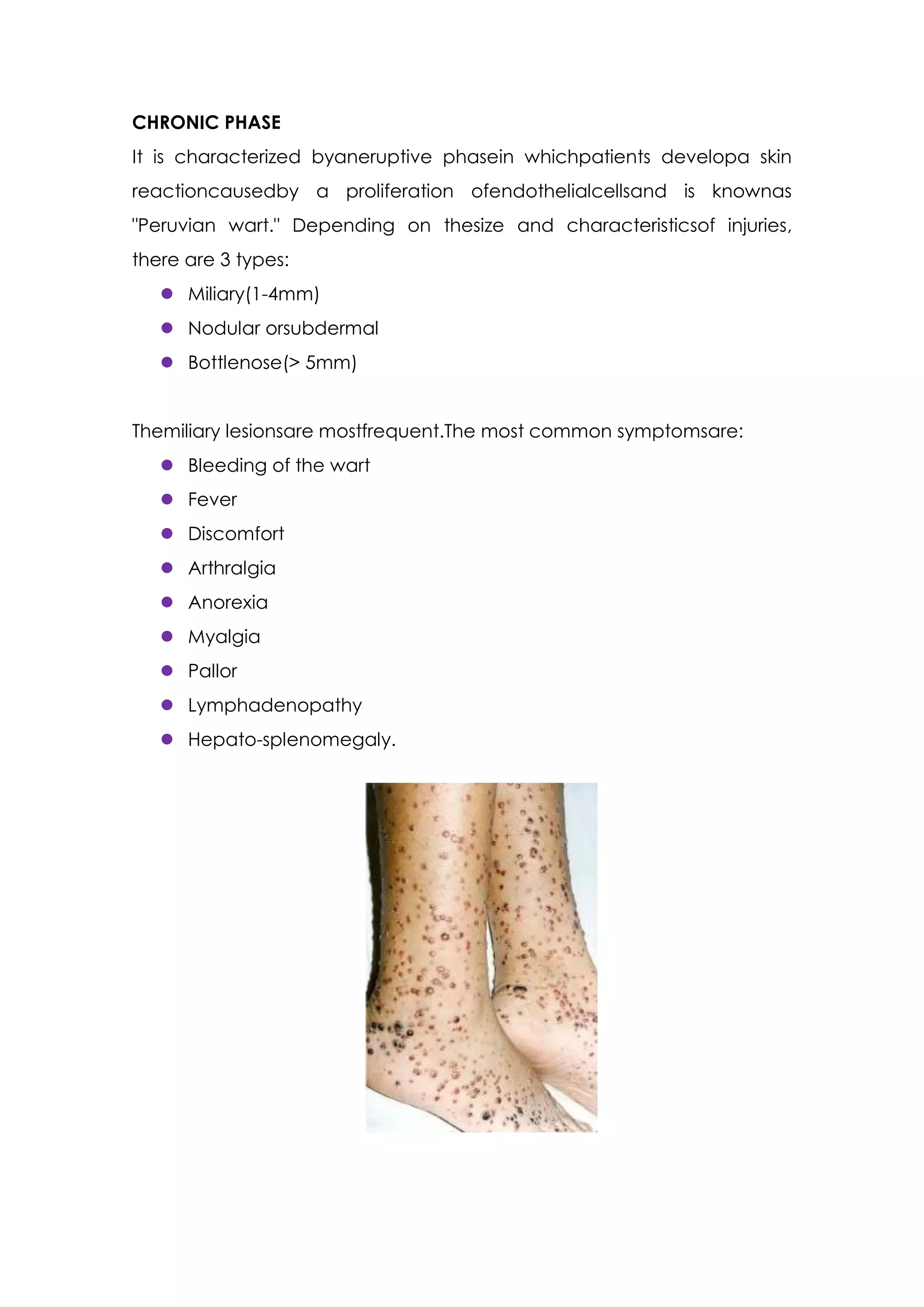
This document discusses bartonellosis, caused by Bartonella bacilliformis infection transmitted by sandflies in Peru, Ecuador, and Colombia. It describes the acute and chronic phases of the disease. The acute phase causes fever, anemia, and potentially fatal complications without treatment. The chronic phase causes skin eruptions known as "Peruvian wart." The document also provides details on diagnosis, treatment with antibiotics, and presents a case report of a patient with acute bartonellosis presenting with fever, jaundice, and complications who was treated with antibiotics and blood transfusions.