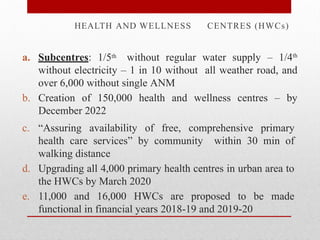
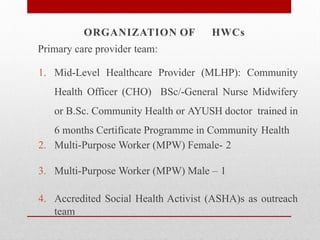
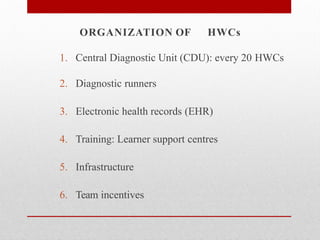
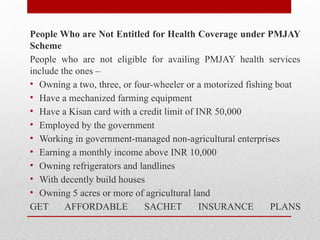
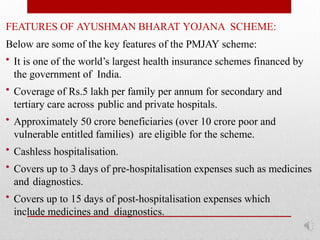
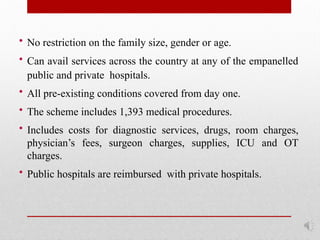
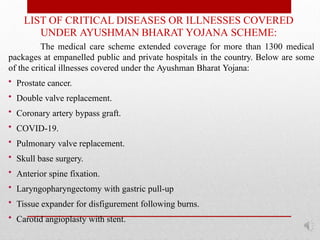
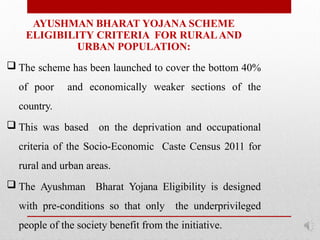
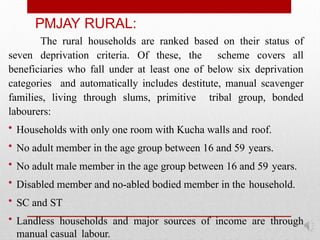
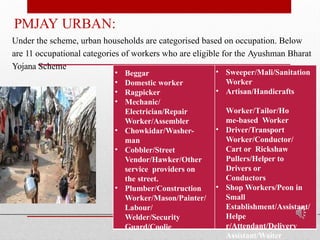
Ayushman Bharat, also known as Pradhan Mantri Jan Arogya Yojana (PM-JAY), is a national health insurance scheme launched in India in 2018 aimed at providing financial protection for hospitalization to the economically weaker sections, covering over 50 crore citizens. It includes two components: the establishment of Health and Wellness Centres for preventive care and the PM-JAY for secondary and tertiary care, offering a cashless coverage of up to ₹5 lakh per family per year. The scheme targets the bottom 40% of the population, ensuring healthcare access to the underprivileged while being fully funded by the government.