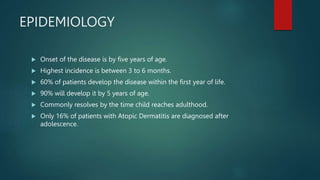
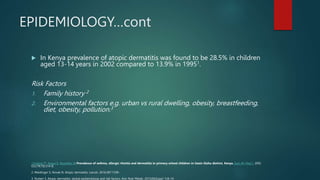
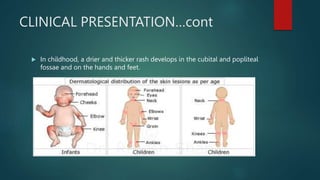
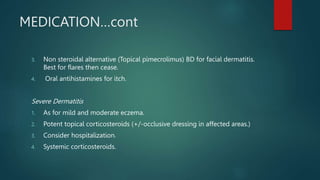
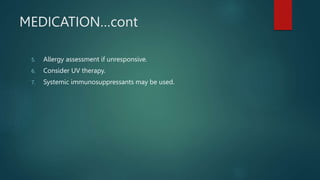
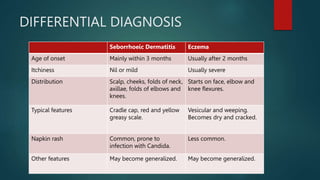
The document provides a comprehensive overview of atopic dermatitis (eczema), including its definition, epidemiology, clinical presentation, and management strategies. It notes that the disease usually presents by age five, with common symptoms including itch and dryness, and emphasizes the importance of proper skin care and potential treatments ranging from mild emollients to systemic immunosuppressants for severe cases. Differential diagnosis with conditions such as seborrhoeic dermatitis is also discussed.