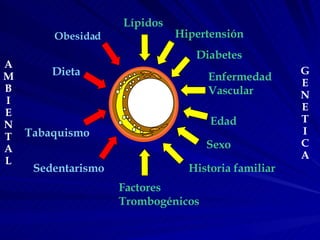
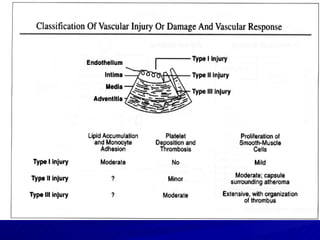
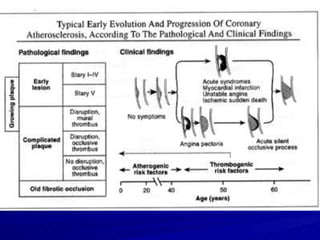
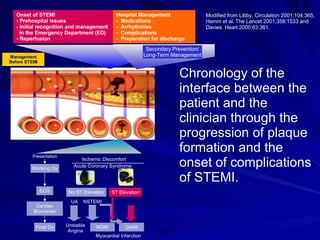
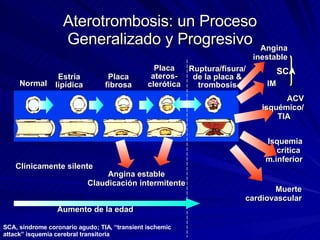
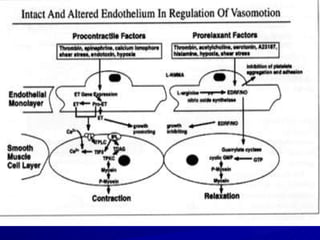
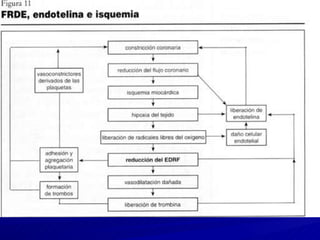
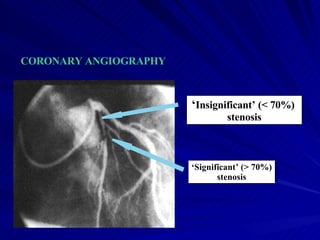
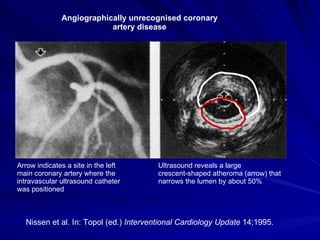
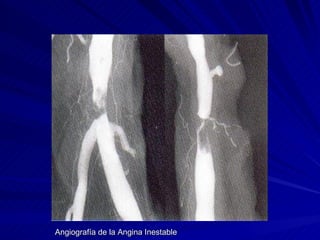
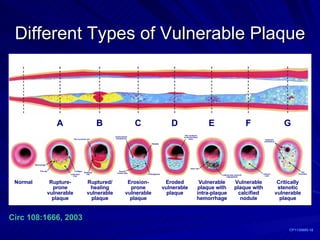
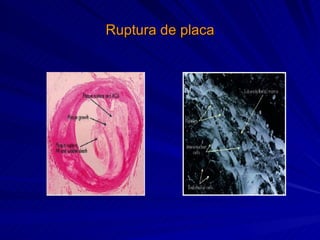
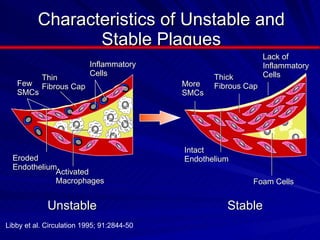
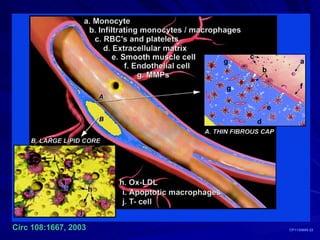
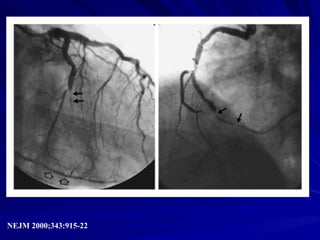
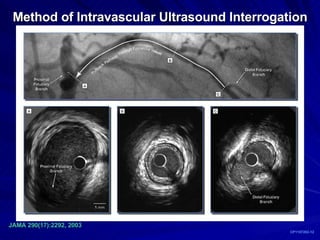
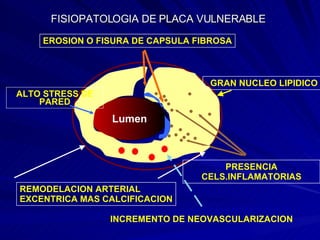
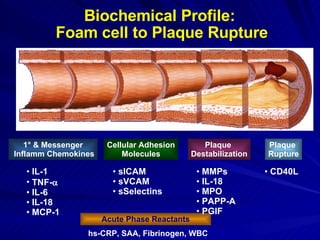
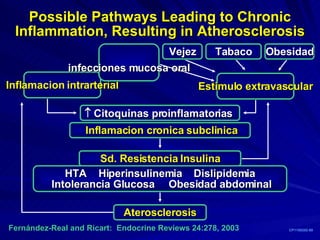
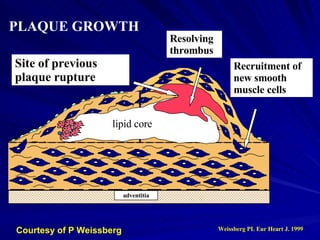
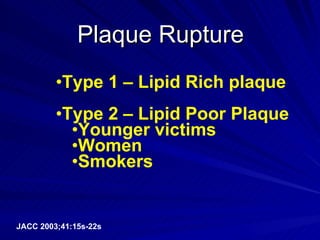
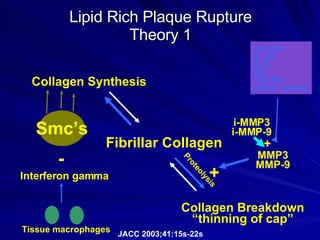
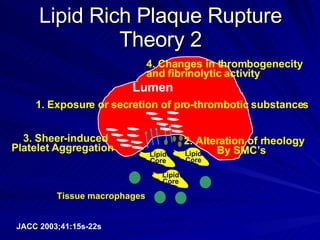
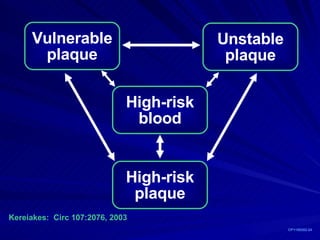
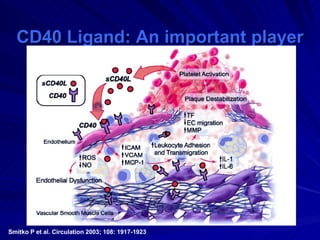
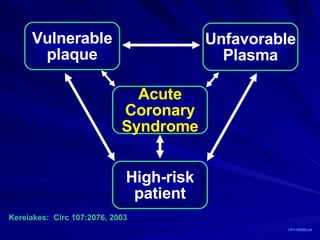
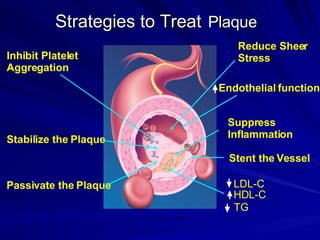
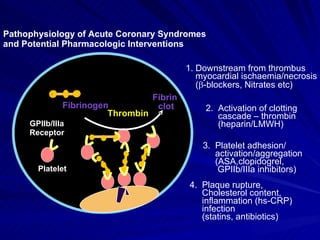
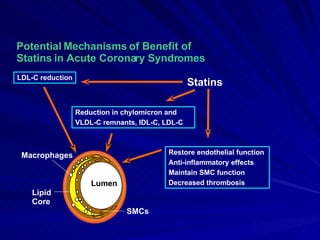
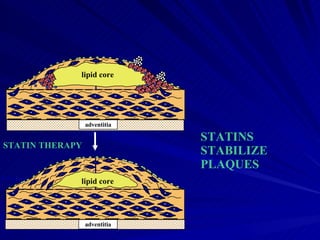
The document discusses atherosclerosis and coronary artery disease. It covers the progression of plaque formation, risk factors for plaque rupture like inflammation, management of acute coronary syndromes like myocardial infarction, and strategies for treating vulnerable plaque including reducing inflammation and cholesterol levels.