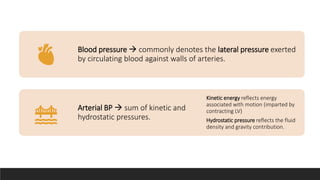
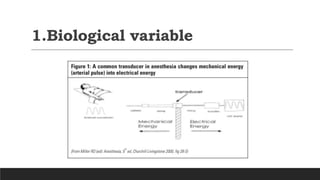
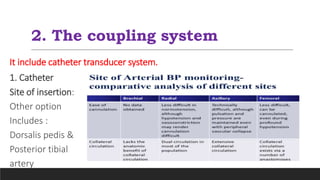
Invasive arterial blood pressure monitoring provides the gold standard for blood pressure measurement. It involves inserting a catheter into an artery using the Seldinger technique. The catheter is connected to a pressure transducer that converts pressure waves into electrical signals. These signals are amplified and processed to display the arterial pressure waveform on a monitor. Dynamic measures like pulse pressure variation and stroke volume variation obtained from the arterial waveform can help assess fluid responsiveness in mechanically ventilated patients. Complications of arterial lines include pain, bleeding, occlusion and infection.

![INTRODUCTION
•Invasive blood pressure monitoring is gold standard
in blood pressure monitoring.
•All the invasive pressure are usually expressed as
mm of mercury except CVP which may be expressed
as cm of water [1mm Hg = 1.36 cm of water].](https://image.slidesharecdn.com/arteriallinecopy-240320085646-2147c149/85/arterial-line-insertion-in-paediatric-practice-3-320.jpg)






























![Stroke volume
variance
•Comparable to SPV
•Arterial line swing
• This phenomenon occurs during
respiration
• Variation of >10% is a sensitive
of fluid responsiveness.
•SPV is a direct reflection of the
stroke volume variation
• SPV = [SP max - SP min / SP mean
1x100]
• SPV >10mmHg is fluid responsive](https://image.slidesharecdn.com/arteriallinecopy-240320085646-2147c149/85/arterial-line-insertion-in-paediatric-practice-41-320.jpg)

![Pulse pressure
variation
•PPV = [Ppmax- Ppmin /
Ppmean ]x 100
•Indicator of the position on
the Frank-Starling curve.
•PPV ≥ 12% is suggestive of
fluid responsiveness.](https://image.slidesharecdn.com/arteriallinecopy-240320085646-2147c149/85/arterial-line-insertion-in-paediatric-practice-43-320.jpg)