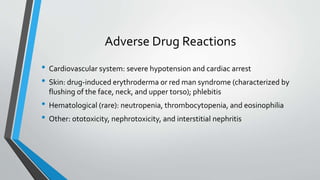
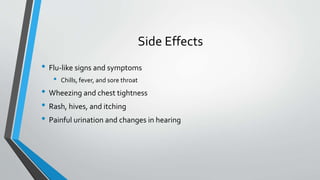
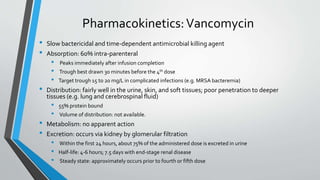
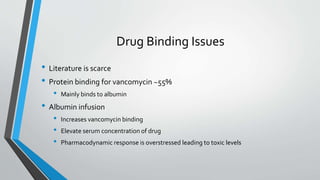
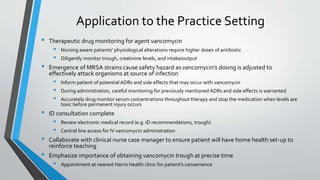
This document is an application paper for a clinical pharmacology course that discusses vancomycin. It summarizes the role of vancomycin in treating MRSA bacteremia and outlines key aspects of vancomycin including its pharmacokinetics, potential drug interactions, adverse effects, and monitoring considerations for patients discharged home on long-term IV vancomycin therapy. The application of vancomycin monitoring and education is discussed for the clinical practice setting.