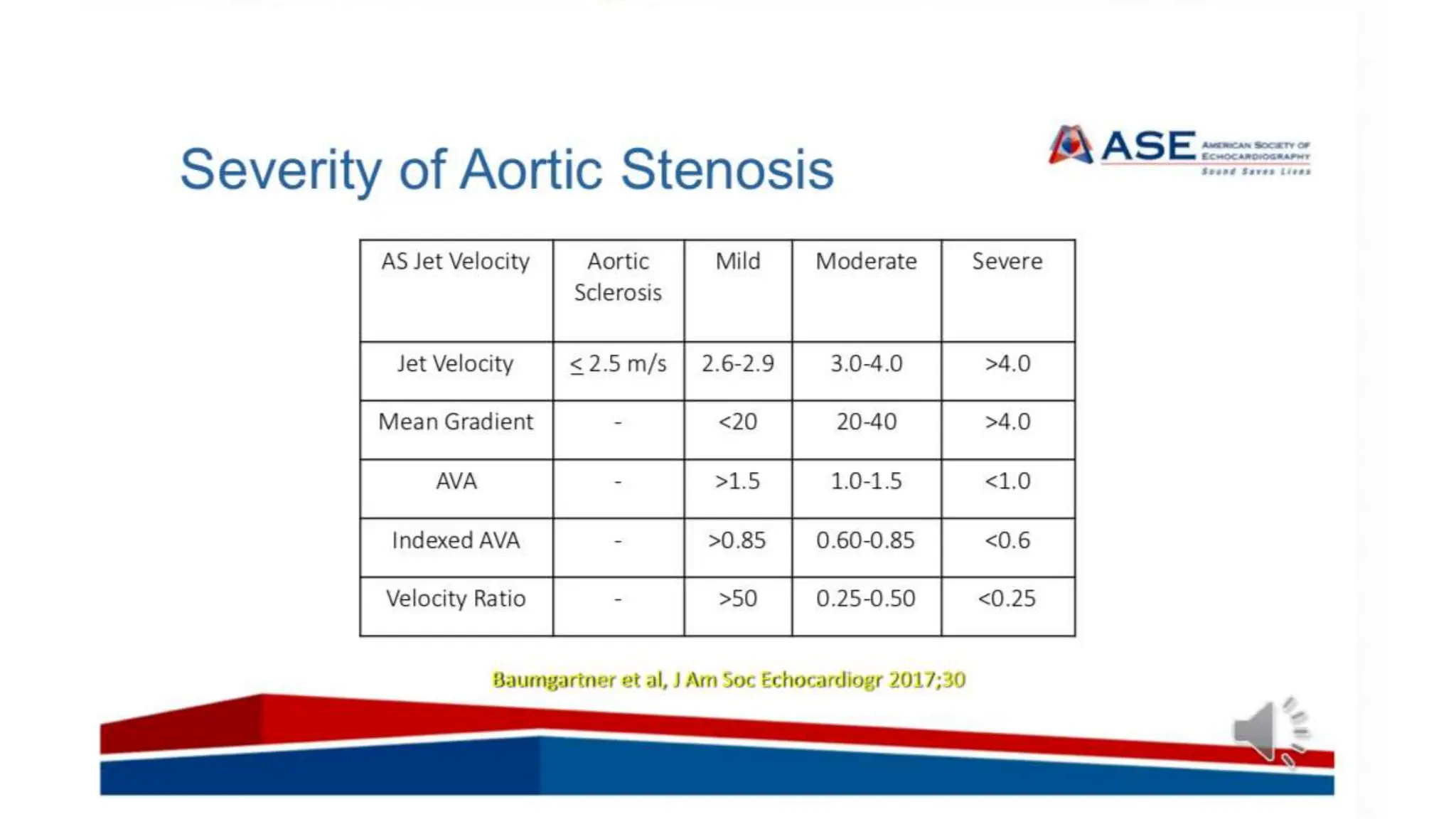
The document provides guidelines for echocardiographic assessment of aortic stenosis (AS), focusing on anatomical evaluation and hemodynamic parameters. It outlines the methods for diagnosing AS severity, including Doppler measurements, flow calculation, and considerations for different patient subgroups. Additionally, it emphasizes the importance of identifying potential confounding factors that may affect the accuracy of AS evaluations.