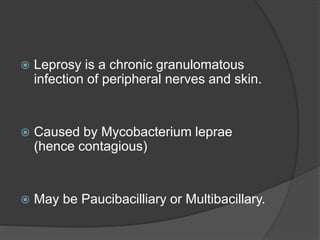
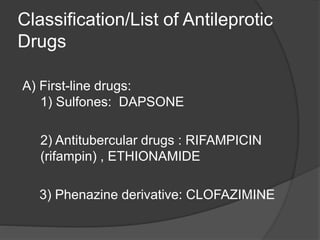
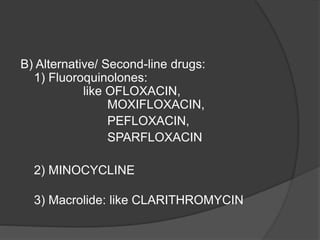
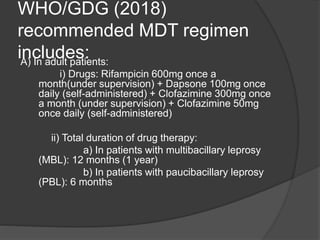
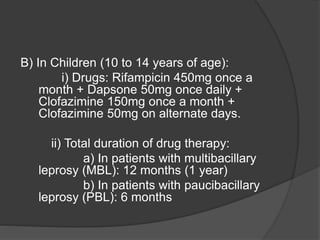
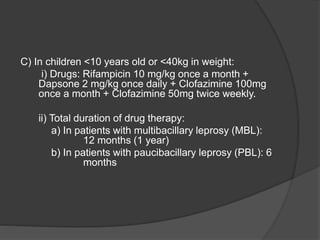
This document summarizes information about the treatment of leprosy. It discusses that leprosy is caused by Mycobacterium leprae and can be successfully treated with multidrug therapy combinations, though nerve damage cannot be reversed. Dapsone is one of the first-line drugs used along with rifampicin and clofazimine according to the WHO recommended multidrug therapy regimen, which involves taking these drugs for either 6 months for paucibacilliary leprosy or 12 months for multibacilliary leprosy. The document also outlines dosing guidelines for both adults and children.