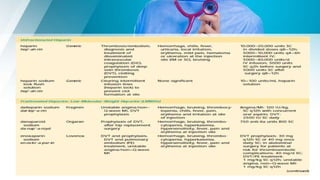
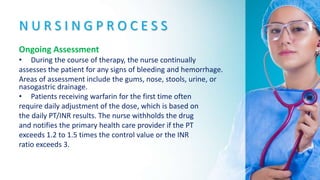
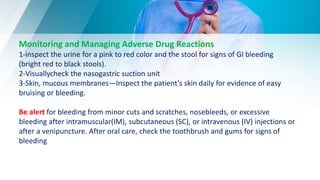
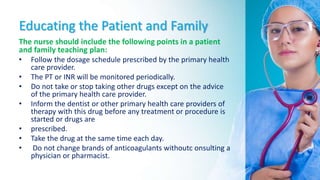
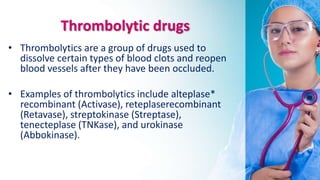
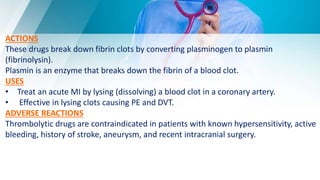
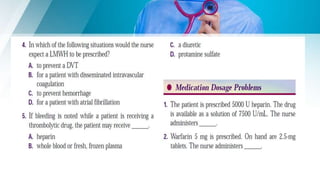
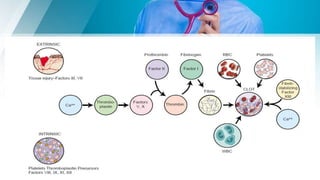
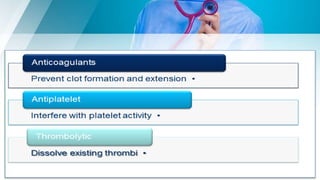
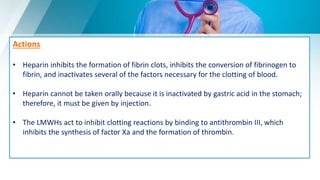
This document summarizes anticoagulant and thrombolytic drugs including heparin, warfarin, and thrombolytic drugs. It discusses their uses, mechanisms of action, adverse effects, interactions, and nursing considerations for assessment and administration. Specifically, it notes that heparin prevents clotting by inhibiting thrombin formation while warfarin interferes with vitamin K-dependent clotting factor synthesis. Ongoing monitoring of coagulation tests is important when administering these drugs to minimize bleeding risks and optimize dosing.



![Uses
Heparin is used for:
• Prevention and treatment of venous thrombosis, PE.
• Atrial fibrillation with embolus formation.
• Prevention of postoperative venous thrombosis(DVT) and PE in certain patients
undergoing surgical procedures, such as major abdominal surgery Prevention of clotting in
arterial and heart surgery, in blood transfusions and dialysis procedures, and in blood
samples for laboratory purposes
• Prevention of a repeat cerebral thrombosis in some patients who have experienced a
stroke
• Treatment of coronary occlusion, acute MI, and peripheral arterial embolism
• Prevention of clotting in equipment used for extracorporeal(occurring outside the body)
circulation
• Maintenance of patency of IV catheters (very lowdoses of 10 to 100 units [U]).](https://image.slidesharecdn.com/anticoag-191024101135/85/Anticoaglant-12-320.jpg)