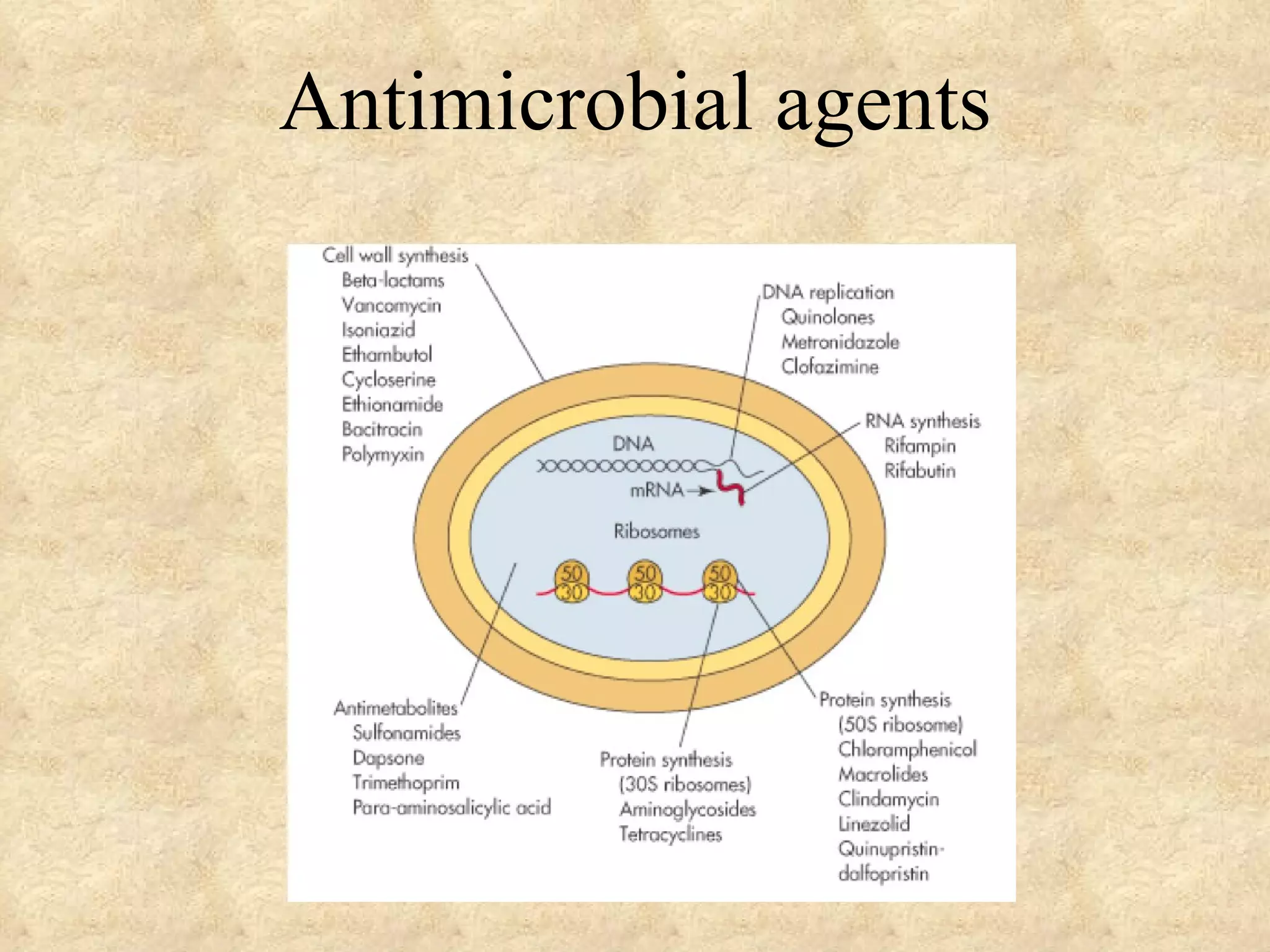
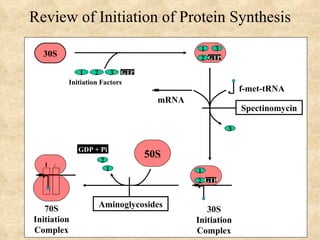
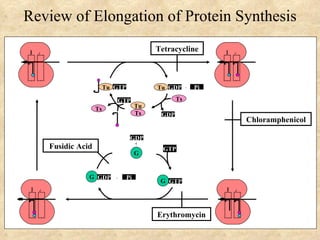
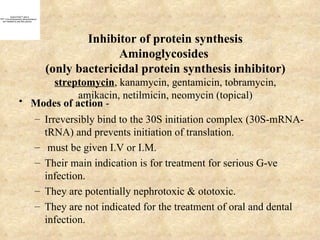
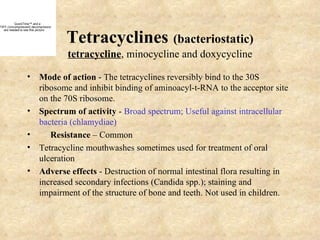
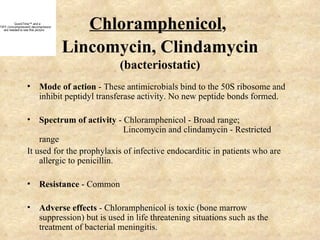
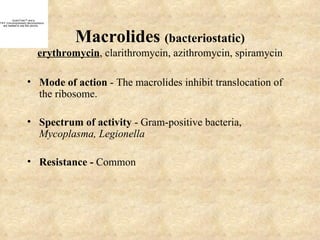
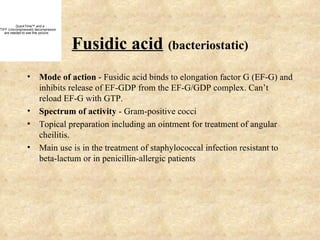
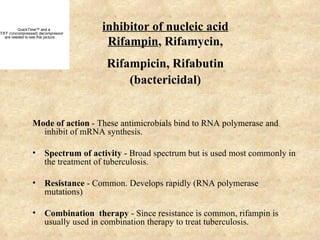
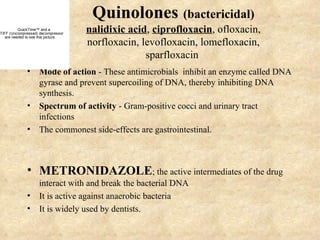
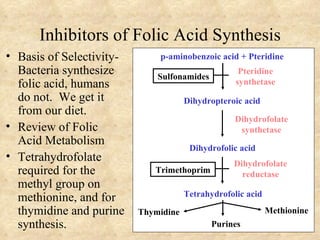
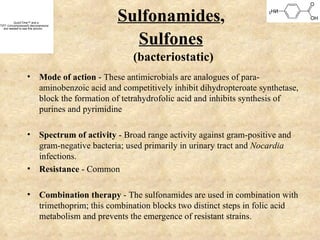
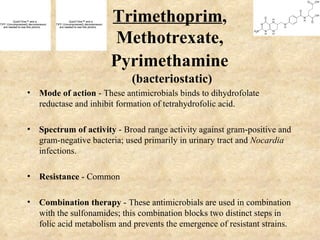
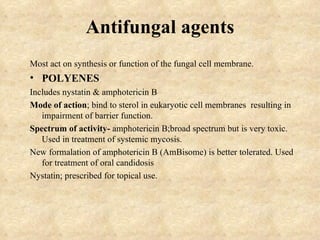
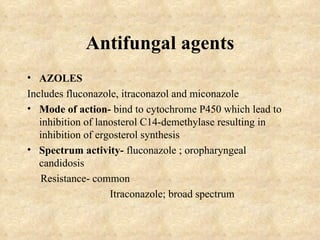
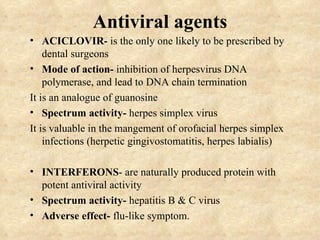
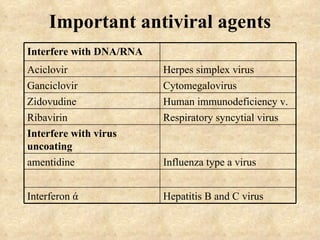
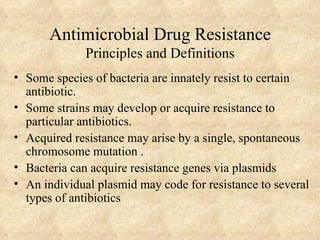
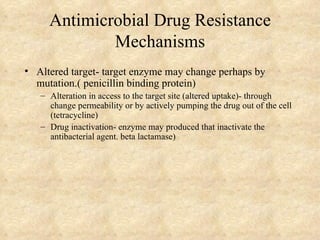
The document discusses various classes of antimicrobial agents including their mechanisms of action, spectra of activity, and examples. It covers antibiotics that inhibit cell wall synthesis, protein synthesis, and nucleic acid synthesis. Resistance mechanisms are also reviewed, including alteration of drug targets, decreased drug access, and drug inactivation.