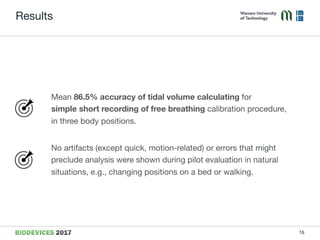
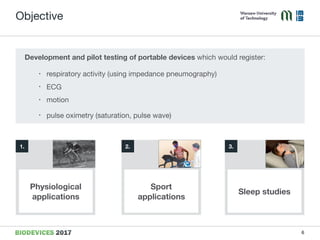
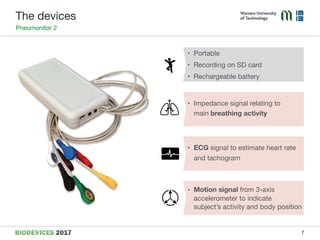
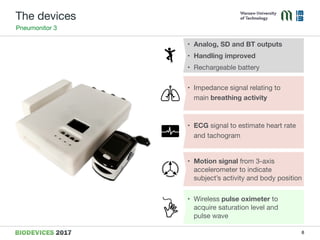
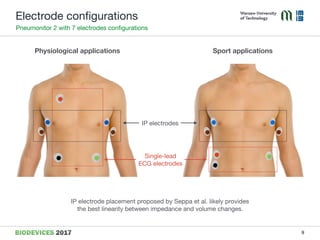
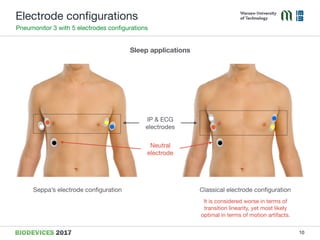
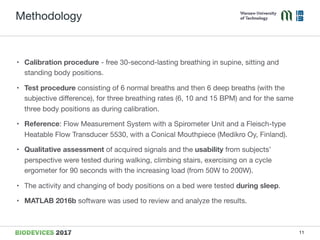
The document discusses the development and testing of portable ambulatory devices designed to measure cardiorespiratory activity, including respiratory patterns and heart activity, using impedance pneumography. It describes two devices, Pneumonitor 2 and Pneumonitor 3, intended for physiological analysis and sleep studies, respectively, highlighting their features and calibration methods. Results indicate that the devices achieve high accuracy in tidal volume calculation and are effective in natural settings, such as during sleep and physical activity.
![Methodology
Subjects - generally healthy students, 10 males
12
Minimum Mean Maximum
Weight [kg] 65.0 77.4 100.0
Height [cm] 171.0 179.3 187.0
BMI 20.75 24.14 33.41
Age 19 23 27](https://image.slidesharecdn.com/biodevices5mlynczak-170227231215/85/Ambulatory-Devices-Measuring-Cardiorespiratory-Activity-with-Motion-12-320.jpg)