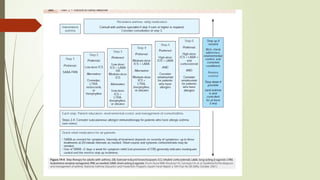
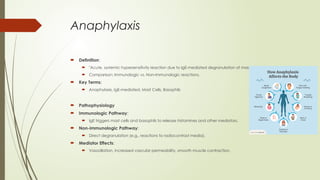
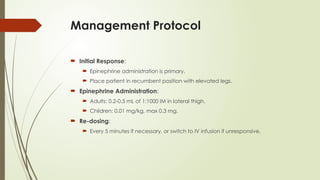
The document provides an extensive overview of allergic diseases, defining conditions such as allergic rhinitis, asthma, and anaphylaxis, along with their symptoms, diagnosis, and management options. Key points highlight the roles of cytokines in exaggerated immune responses, differentiation between allergic and non-allergic conditions, and various treatment strategies including medications and immunotherapy. Emphasis is placed on the importance of rapid diagnosis and intervention, particularly in cases of anaphylaxis, where epinephrine administration is critical.