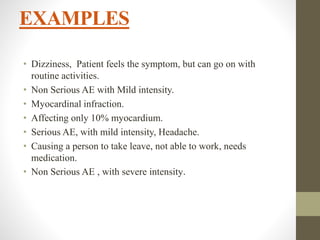
The document presents an overview of pharmacovigilance, focusing on the detection, assessment, understanding, and prevention of adverse effects related to medicinal products. It defines adverse events and drug reactions, categorizing them by severity and reporting responsibilities for investigators and sponsors in clinical research. Critical reporting timelines and procedures for serious adverse drug reactions are also outlined.
![WHO definition of
pharmacovigilance
It is the science and activities relating to the detection, assessment,
understanding and prevention of adverse effects or any other
medicine related problem.
1] Detection
2] Assessment and understanding
3] Prevention of adverse effects
Pharmacovigilance](https://image.slidesharecdn.com/adverseeventreportingsystemandforms-240518051530-5341a388/85/Adverse-Event-Reporting-system-and-Forms-pptx-2-320.jpg)
![ADVERSE EVENT[AE]
• Any unfavorable and
unintended sign.
• Including an abnormal
laboratory finding
• Symptom
• Disease
UNWANTED EFFECTS
• Symptoms [headache,
nausea]
• Physical findings [BP,
lump, edema]
• Abnormal lab values
[increased liver enzymes,
decreased hemoglobin]
• Overdoses important to
define what% cut-off to
be taken as adverse
events.](https://image.slidesharecdn.com/adverseeventreportingsystemandforms-240518051530-5341a388/85/Adverse-Event-Reporting-system-and-Forms-pptx-4-320.jpg)
![Adverse drug reaction [ADR]
In the pre-approval clinical experience:
Defined as all noxious and unintented responsed to a medicinal
product related to any dose should be considered adverse drug
reactions.
The phrase ‘ response to a medical products’ means that a casual
relationship between a medicinal product and an adverse event is
at least a reasonable possibility, i.e. relationship can’t be ruled
out.](https://image.slidesharecdn.com/adverseeventreportingsystemandforms-240518051530-5341a388/85/Adverse-Event-Reporting-system-and-Forms-pptx-6-320.jpg)
![CONTT..
UNEXPECTED ADVERSE DRUG REACTION:
An adverse reaction, the nature or severity of which is not
consistent with the applicable product information.
[E.g. Investigator’s brochure for an unapproved investigational
medicinal product]
SERIOUS ADVERSE DRUG REACTION:
• Results in death.
• Life-threatening
• Requires inpatient hospitalization or prolongation of existing.
• Hospitalization.
• Birth defect.](https://image.slidesharecdn.com/adverseeventreportingsystemandforms-240518051530-5341a388/85/Adverse-Event-Reporting-system-and-Forms-pptx-7-320.jpg)
![INTENSITY
• Severity of the Adverse Event [ WHO Classification ]
1.MILD: Awareness of sign, symptom, or event, but easily
tolerated.
2.MODERATE: Discomfort enough to cause interference with
usual activity and may warrant intervention.
3.SEVERE: Incapacitating with inability to do usual activities or
significantly affects clinical status, and warrants intervention
required.](https://image.slidesharecdn.com/adverseeventreportingsystemandforms-240518051530-5341a388/85/Adverse-Event-Reporting-system-and-Forms-pptx-9-320.jpg)
![REPORTING TIME FRAMES
• 1.REGULATORY 2.IRB/IEC 3.PARTICIPATING
INVESTIGATORS
• Serious Unexpected Fatal or Life-threatening unexpected
ADRs
• Fatal or life-threatening, unexpected ADRs occurring in
clinical investigations qualify for every rapid reporting.
• Regulatory agencies should be notified [e.g. By telephone ,
facsimile transmission, or in writing] as soon as possible but
no later than 7 calendar days after first knowledge by the
sponsor that a case qualifies, followed by within 8 additional
calendar days the complete report.
• This report should include an assessment of the importance
and implication of the findings including relevant previous
experience with the same or similar medicinal products.](https://image.slidesharecdn.com/adverseeventreportingsystemandforms-240518051530-5341a388/85/Adverse-Event-Reporting-system-and-Forms-pptx-11-320.jpg)
