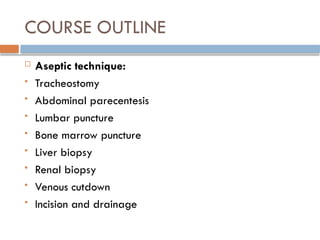
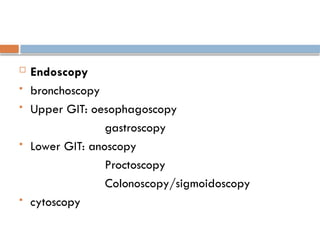
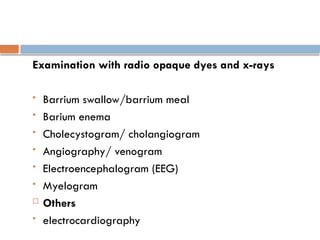
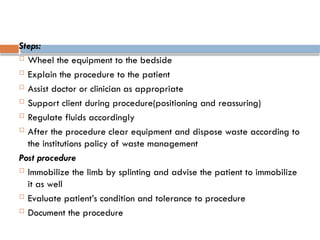
The document outlines advanced nursing procedures including tracheostomy, abdominal paracentesis, lumbar puncture, bone marrow biopsy, liver biopsy, and renal biopsy, detailing indications, procedures, and required nursing care. Each procedure includes preparation steps, nursing actions post-procedure, and potential complications to monitor. By the end of the course, students should demonstrate an understanding of aseptic techniques and effective patient management before, during, and after these procedures.