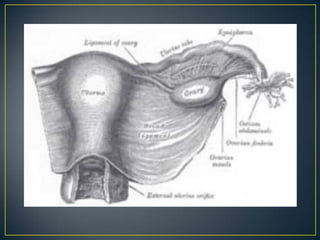
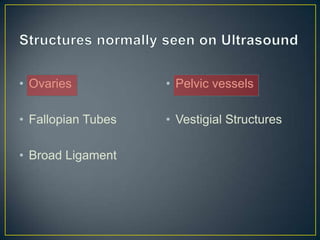
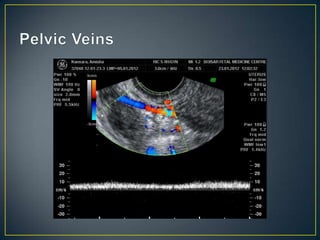
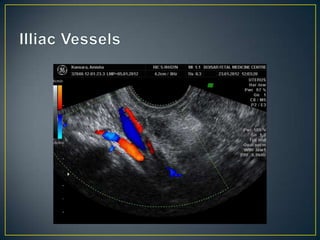
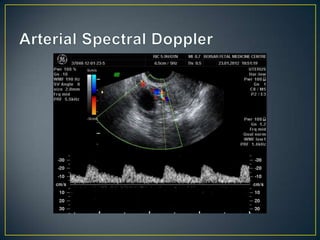
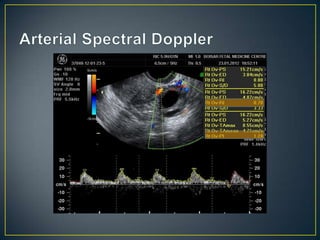
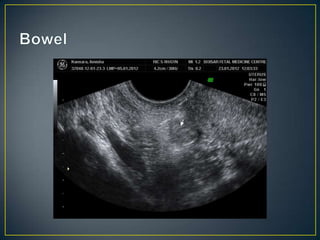
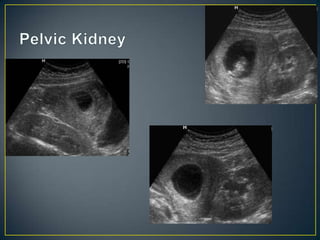
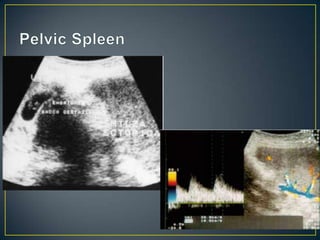
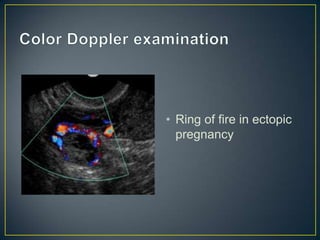
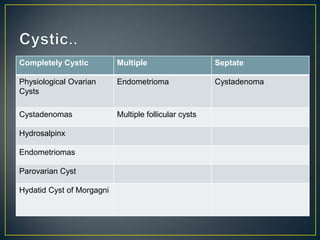
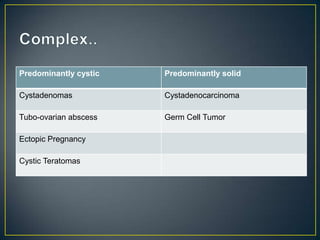
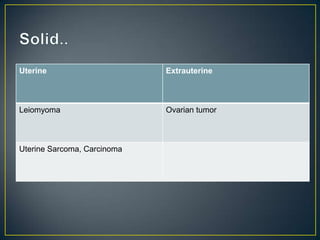
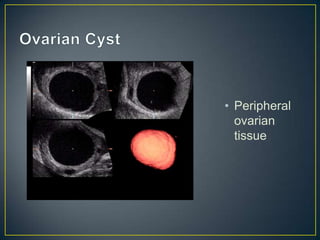
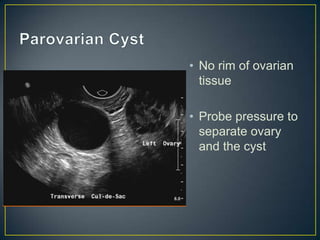
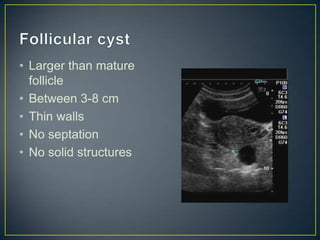
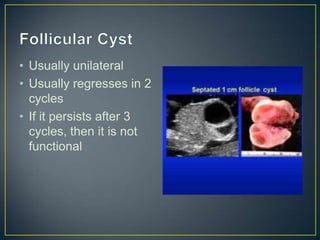
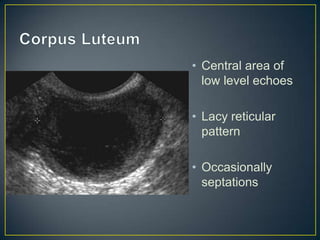
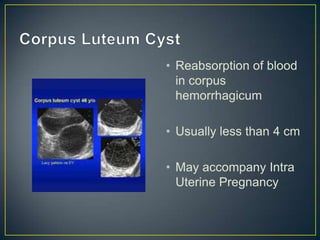
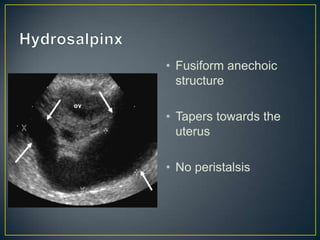
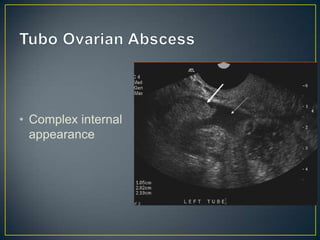
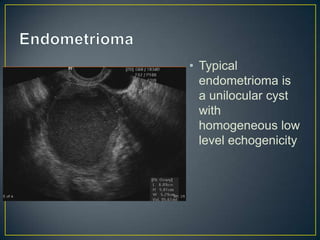
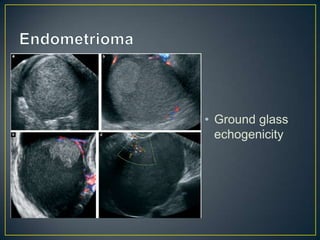
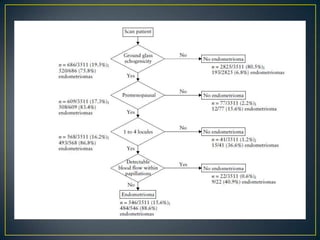
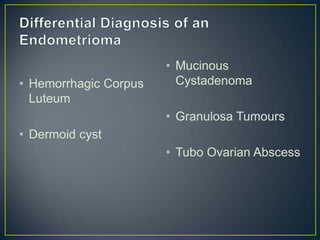
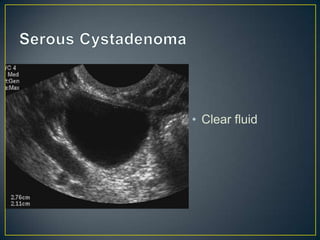
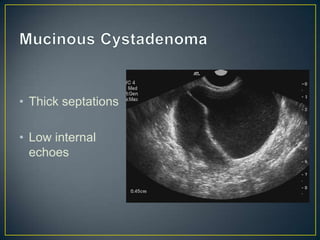
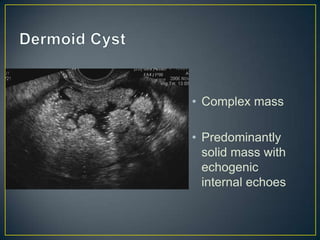
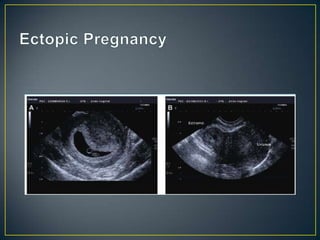
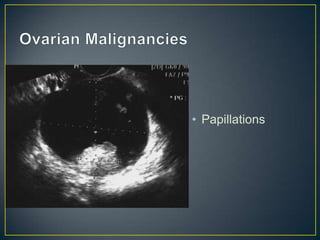
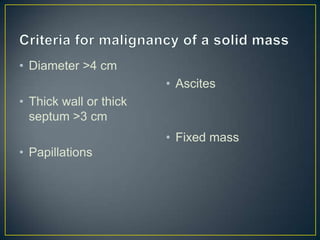
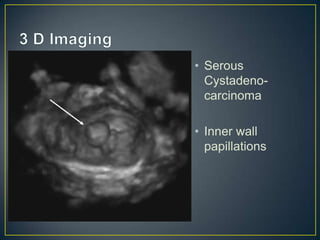
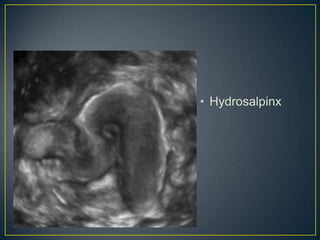
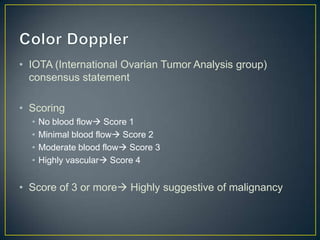
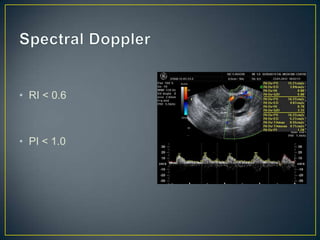
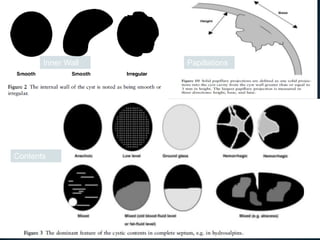
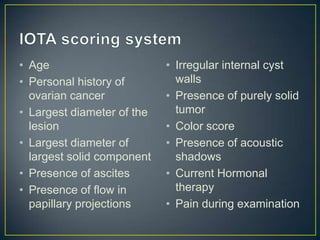
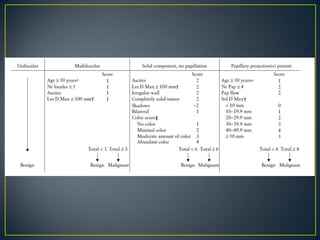
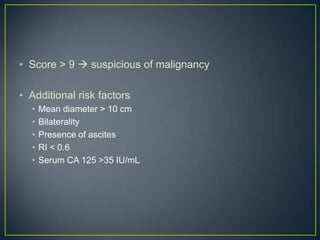
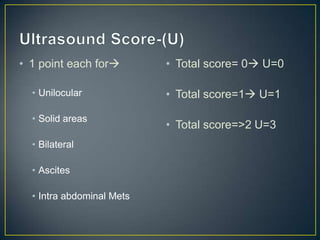
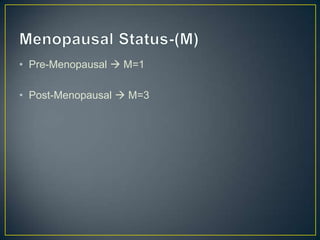
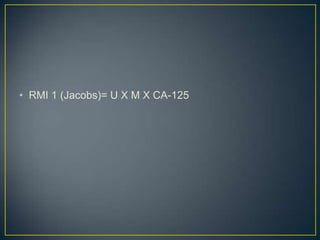
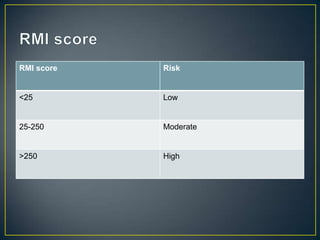
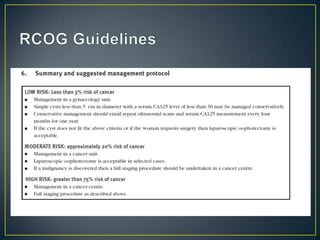
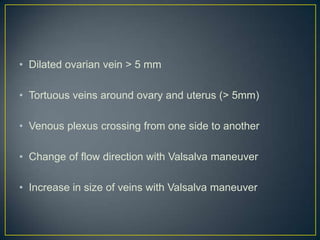
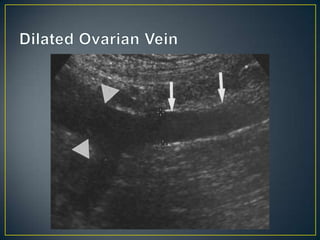
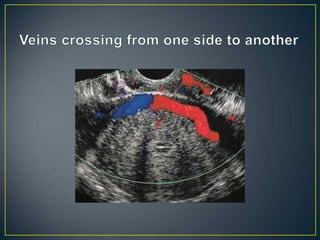
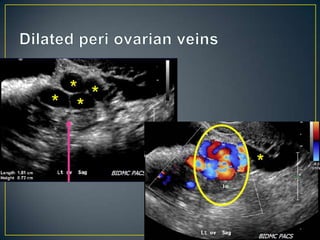
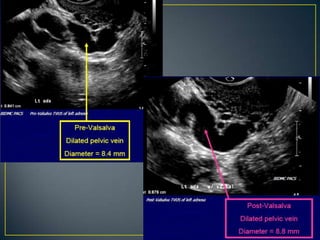
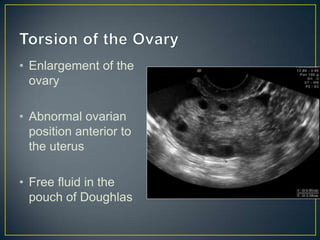
The document provides guidelines for pelvic ultrasound examination. It describes evaluating the ovaries and using them as reference points. If pathology is seen, its size and sonographic features should be documented. Spectral Doppler should be performed to examine vessels. The fallopian tubes and other structures should also be examined. Characteristics of different types of ovarian cysts and masses are outlined. The document also discusses features suggestive of malignancy on ultrasound and risk of malignancy indices.