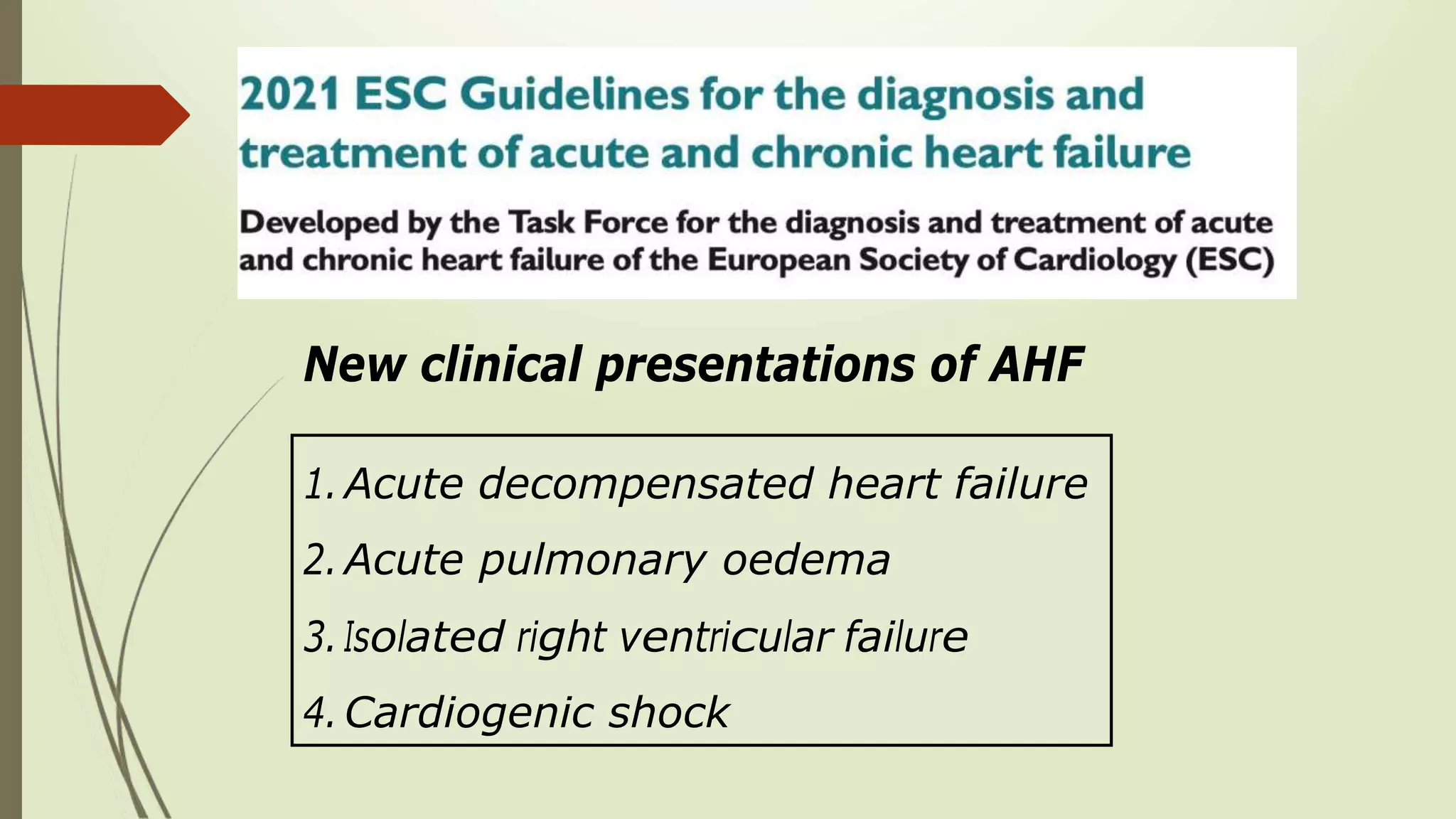
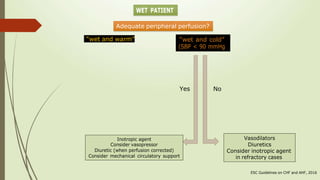
1. New clinical presentations of acute heart failure (AHF) include acute decompensated heart failure, acute pulmonary edema, isolated right ventricular failure, and cardiogenic shock.
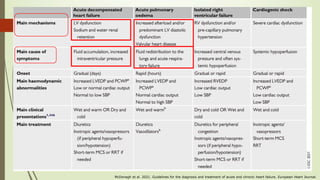
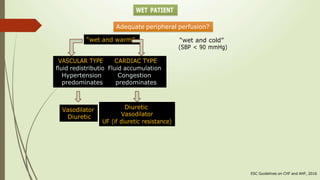
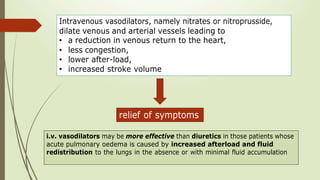
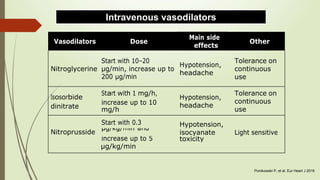
2. Intravenous vasodilators such as nitrates and nitroprusside are recommended to reduce congestion and afterload in AHF patients with increased filling pressures and fluid redistribution to the lungs.
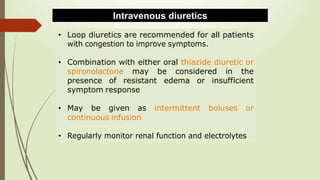
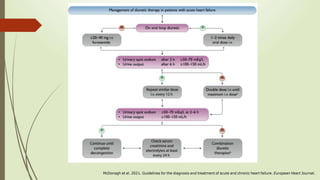
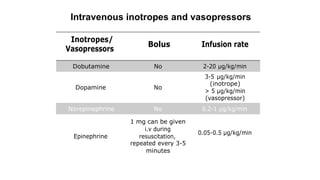
3. Intravenous loop diuretics are recommended for all AHF patients with congestion to improve symptoms, and thiazide diuretics or spironolactone can be added for resistant edema. Inotropic agents may be considered for refractory cases.