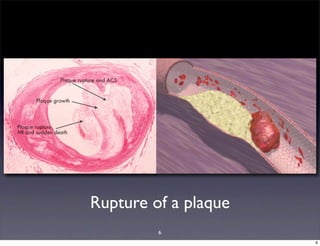
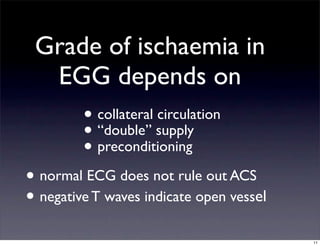
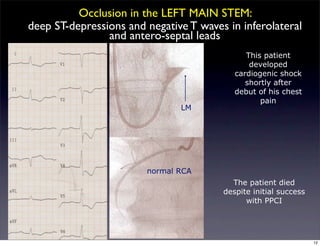
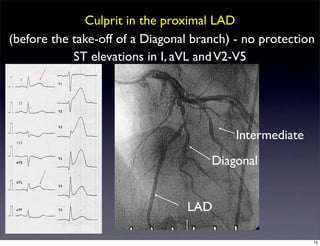
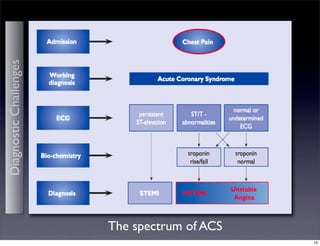
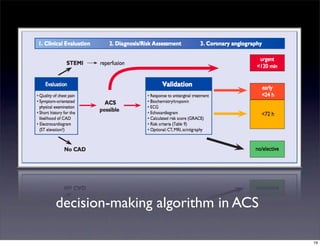
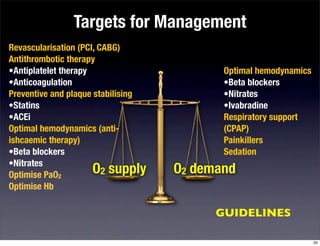
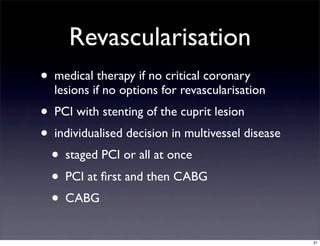
This document discusses the diagnostic challenges of acute coronary syndrome (ACS) including atypical presentations in older patients, women, and those with other conditions. It outlines the pathophysiology of ACS from plaque rupture and thrombus formation, which can decrease blood flow and cause myocardial hypoxia and ischemia. Diagnosis involves evaluating the electrocardiogram, markers of myocardial injury, and risk factors. Treatment focuses on optimizing oxygen supply and demand through revascularization, antiplatelet/anticoagulation therapy, and managing hemodynamics and comorbidities. The guidelines provide targets and algorithms for managing ACS patients.