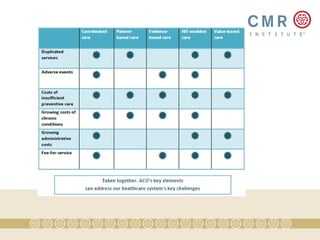
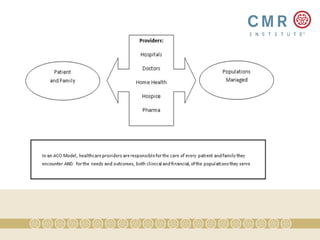
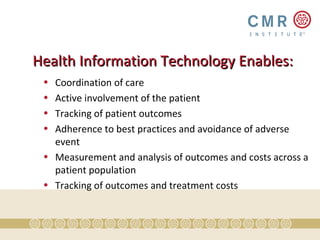
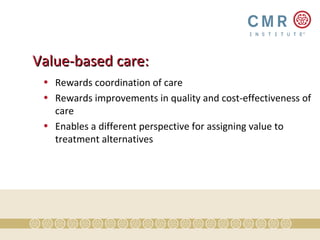
Accountable Care Organizations (ACOs) aim to enhance healthcare value by managing costs and improving quality through coordinated, patient-centered care across various providers. The ACO model emphasizes five key elements: coordinated care, patient-centered care, evidence-based practices, health information technology, and value-based payment. By integrating these elements, ACOs can reduce inefficiencies, improve patient outcomes, and foster accountability in healthcare delivery.