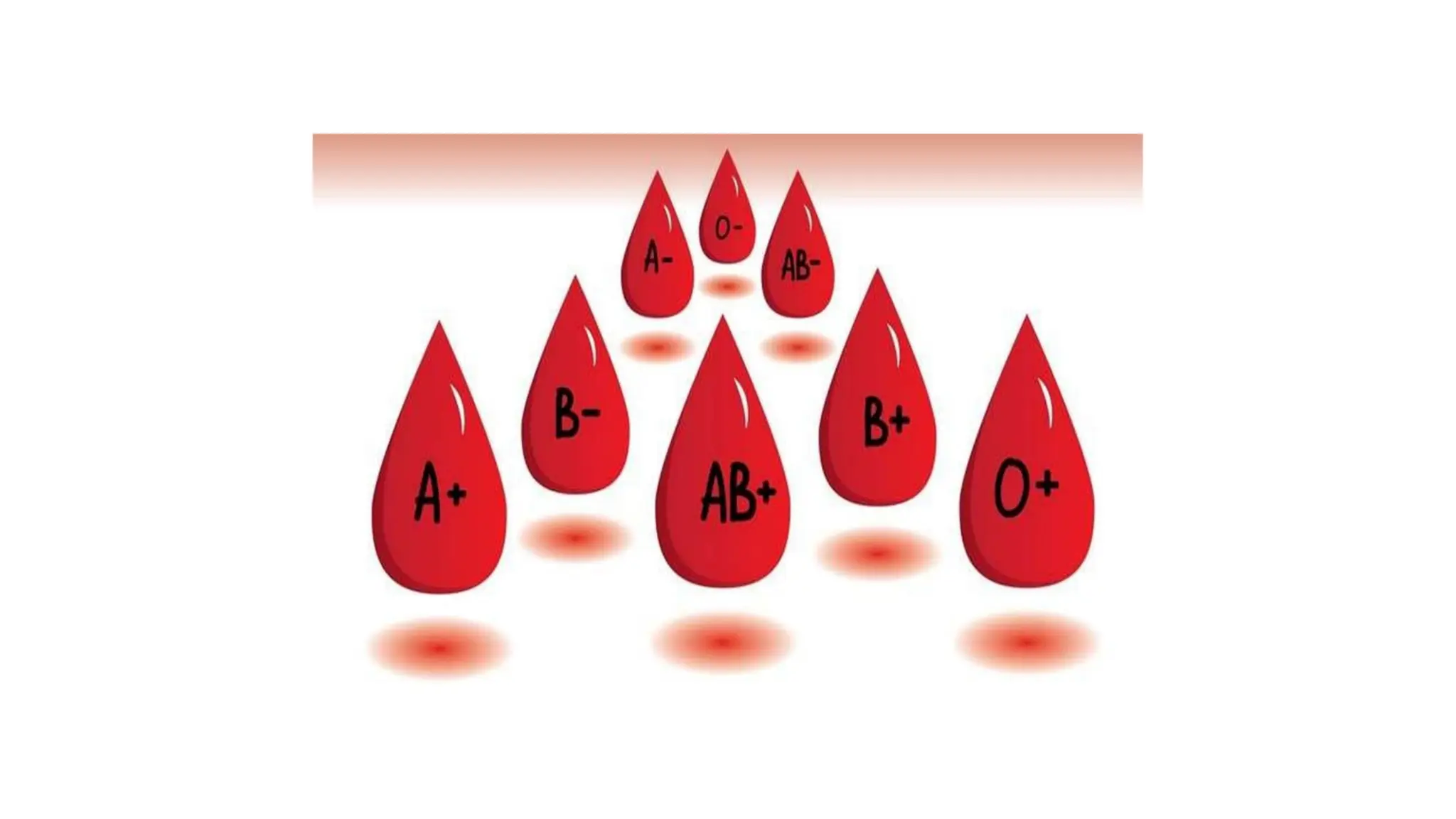
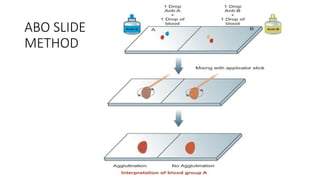
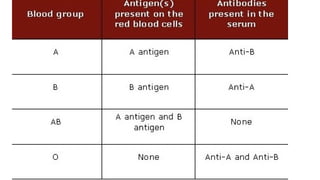
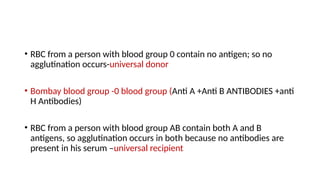
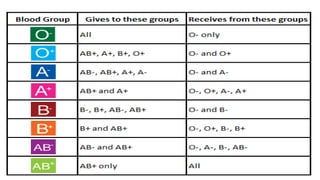
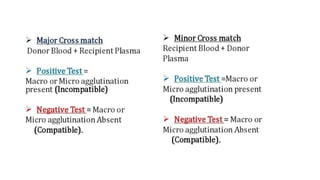
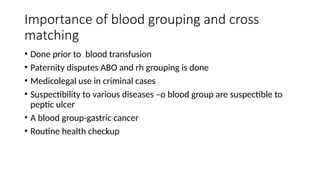
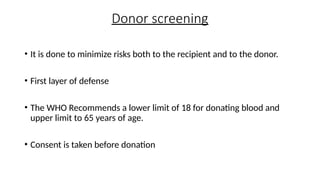
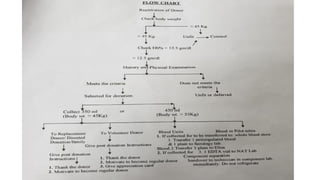
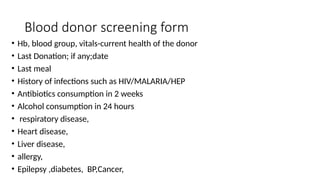
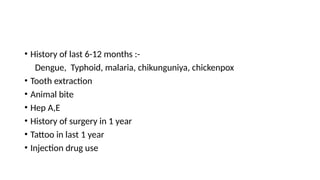
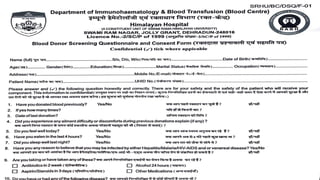
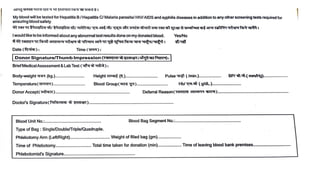
The document discusses blood group systems including the ABO and Rh systems, detailing how blood types are determined based on the presence of antigens and antibodies. It explains the compatibility tests required before blood transfusions to prevent adverse reactions, as well as the importance of blood grouping for medical and legal purposes. Additionally, it outlines the blood donor screening process to ensure donor and recipient safety.