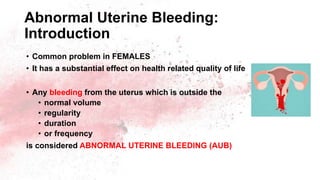
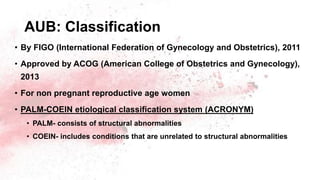
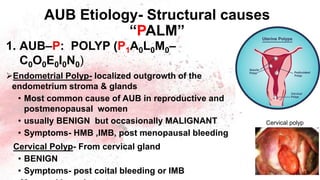
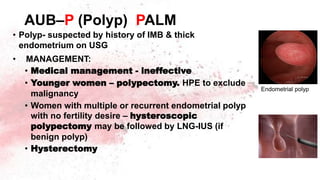
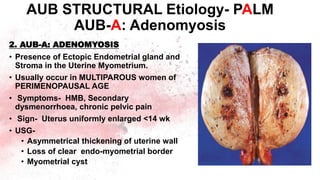
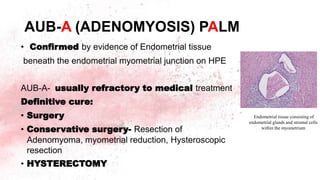
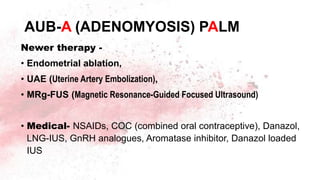
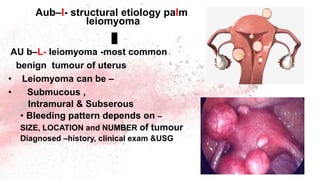
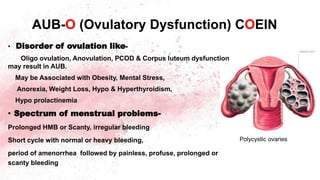
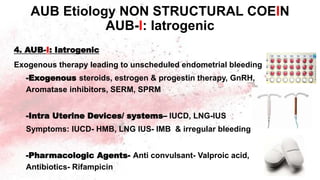
Abnormal uterine bleeding is a common gynecological problem that can affect women of all ages. It is defined as bleeding outside of normal menstrual parameters of volume, regularity, duration, and frequency. The document outlines the normal menstrual cycle and parameters of abnormal bleeding. It then describes the PALM-COEIN classification system for etiologies of abnormal uterine bleeding, including structural causes like polyps, adenomyosis, and leiomyomas (PALM) and non-structural causes like coagulopathies, ovulatory dysfunction, and endometrial factors (COEIN). Evaluation and management approaches are discussed for each etiology.

![3. AUB-L: LEIOMYOMA
• Subclassified as
- those with at least ONE Submucous
leiomyoma, AUB-L-SM and
- those having NO Submucous
leiomyoma AUB-L-O [OTHER]
• Commonest cause of AUB in
Reproductive age
• Symptoms- HMB, IMB, irregular
bleeding
AUB STRUCTURAL Etiology- PALM
AUB-L: Leiomyoma](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-23-320.jpg)
![.Other cancer of genital tract – may present
with AUB
• Cervical cancer –Occur in younger age [mid
40s], associated with IMB, PCB
• Vulval, Vaginal cancer- RARE, but can present
with bleeding
AUB-M (Malignancy and hyperplasia)
PALM
Cervical Cancer](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-28-320.jpg)
![Contd..
Pathogenesis: ANOVULATION
• Low level of oestrogen→ No LH surge → NO OVULATION → NO corpus
luteum formation → NO PROGESTERON production → Decrease level of
PGF2α, other PGs & Thrombxanes → Increase Fibrinolysis → Painless
bleeding [no vasoconstrict]
• Presence of developing follicle → prolonged supply of Estrogen →
Endometrial proliferation & Hyperplasia → Fragile Endometrial with no
stromal support → continuous prolonged bleeding followed by → amenorrhea
AUB-O (Ovulatory Dysfunction) COEIN
No LH Surge
No ovulation
No corpus luteum
No progesterone
→](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-34-320.jpg)
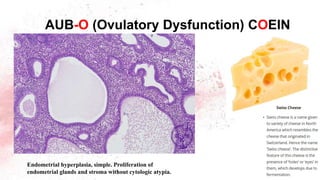
![May be associated with –
- Follicular cyst of the ovary
- Endometrial hyperplasia
Prolonged amenorrhea- Endometrium shows CYSTIC
HYPERPLASIA, [SWISS CHEESE appearance]
“Metropathia hemorrhagica”, “Schroeder’s disease”
• Characteristic
- Hyperplastic gland &stroma
- Cystic or irregularly dilated gland
- Increase in Vascularization
- Necrosis of Superficial Endometrium
- Tortuous & Dilated SPIRAL ARTERIOLES and veins
AUB-O (Ovulatory Dysfunction) COEIN](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-35-320.jpg)
![• Combined Oral Contraceptive [COC]–first line treatment if
pregnancy not desired
• Cyclical Progesterone therapy-
• Cyclical Norethisterone for 21 days [day5 -25 ]x 3 cycle
• Cyclical Progestin luteal phase- for 10-14 days [ 15-25 ]-3
cycle
• LNG-IUS
Adolescent –both & Hormonal & non Hormonal treatment
AUB-O (Ovulatory Dysfunction) COEIN](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-37-320.jpg)
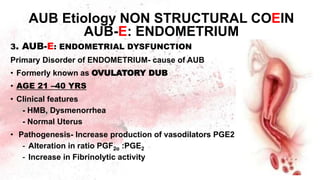
![• Diagnosis of EXCLUSION- after ruling out other identifiable abnormalities
in women with normal ovulatory cycle
• HPE: Endometrium reveals SECRETORY changes as OVULATION &
PROGESTERON normal
• Management: same as AUB –O, but only 21 days therapy is effective
• Chronic inflammation of the ENDOMETRIUM with or without associated
PID- Uncommon cause of AUB
AUB-E (ENDOMETRIAL Dysfunction)
COEIN
DUB may or may not be associated with OVULATION
• Anovular bleeding- 80%: AUB-O [Anovulatory DUB]
• Ovular bleeding - 20%: AUB-E [Ovulatory DUB]](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-39-320.jpg)
![5. AUB-N: Not yet classified/ ill defined cause
- Congenital or acquired A-V Malformation
- Caesarean scar Defect
- Endometrial pseudo aneurysm
- Chronic Endometritis
• Treatment-
• Hormonal: LNG-IUS, COC
• A-V Malformation- Uterine Artery Embolization
• Non Hormonal- NSAID, Tranexamic acid
• GnRH Agonist with ADD-BACK therapy
• Conservative surgery[Ablation] & Hysterectomy- last resort
AUB Etiology NON STRUCTURAL -COEIN
AUB-N: Not yet classified
All these can cause AUB](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-42-320.jpg)
![AUB: Investigation –LAB testing
• Complete blood count [CBC] –for all
• Coagulation profile- platelet count, Bleeding time
• Prothrombin time ,partial thromboplastin time
• - Indicated in all young girl & women with
Positive screen test for coagulopathies
• Testing for –Von Willebrand disease [Hematologist]
• Thyroid function test–young girl, if needed
• Hormonal assay- LH, FSH, TESTOSTERONE,17HP,
Androstenedione, Prolactin level
• Pregnancy test –exclude](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-46-320.jpg)
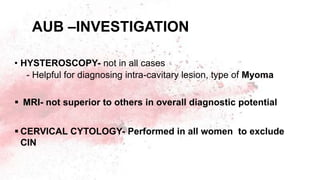
![AUB : Investigation -IMAGING
• ULTRASOUND – Evaluate: UTERUS, ADENEXA, ENDOMETRIUM
-to help in diagnosis of myoma, polyp, adenomyosis & endometrial
thickness.
• DOPPLER ULTRASONOGRAPHY- In Suspected A-V malformation
- Malignancy & to differentiate between FIBROID &ADENOMYOSIS
• 3D-USG-To evaluate Intra-cavitary & Myometrial lesion
• SALINE INFUSION SONOGRAPHY [SIS]- Suspected intra-cavitary
lesion e.g. polyp
- USG performed after introduction of saline in to the uterine cavity
[Sonohysterography]](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-47-320.jpg)
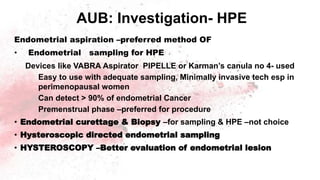
![Aub- investigation--HPE
• Endometrial sampling for Histopathology [HPE]-
Women > 40 yrs
Women < 40yrs –having high risk factor for MALIGNANCY
• Like –Irregular bleeding, obesity, Hypertension, PCOS,
• Endometrial thickness >12mm, Diabetes,
• Family History of Malignancy–ovary, breast ,endometrium, colon
• Use of Tamoxifen
• Late Menopause
• exposure to unopposed estrogen
• AUB –unresponsive to medical therapy](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-48-320.jpg)
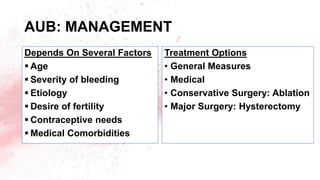
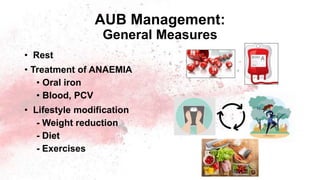
![AUB-COEIN: GENERAL
MANAGEMNET GUIDELINE
• Tranexamic acid- first line therapy. Other non hormonal option- NSAIDs
• LNG-IUS – Desiring Contraception
• COC 2ND LINE therapy
• Cyclical oral Progestin [day 5-26] for 21days T/T of AUB-E
• Cyclical Luteal phase Progestin- orally10-14 days,[ day 15 to 25 ] for
AUB -O
• Ormeloxifene- Saheli: SERM- Where steroids contraindicated
• GnRH agonist with Add-back hormone- last resort
• Endometrial Ablation- if failure to medical or high risk for hysterectomy.-
Endo-Ablation replaced by LNG-IUS
• All AUB pts- HAEMATINICS to prevent ANAEMIA](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-59-320.jpg)
![AUB MANAGEMENT: ACUTE
BLEEDING
• Treatment relies on- Etiology of bleeding, medical problem, fertility
desire & clinical stability. Pregnancy-EXCLUDE
• Medical therapy- Tranexamic acid, oral/ iv- 500- 1000mg [4gm/d]
• Progestin- oral norethisterone, Medroxyprogesterone- high dose
• COC (Combined Oral Contraceptive) cascade
• Conjugated equine estrogen iv 25 mg 4hrly
• Hospitalization – if unstable & serious
• Treat Anaemia](https://image.slidesharecdn.com/abnormaluterinebleedinglinkind-220715165349-5bfe9a43/85/Abnormal-uterine-bleeding-linkind-pptx-66-320.jpg)