Embed presentation
Download to read offline

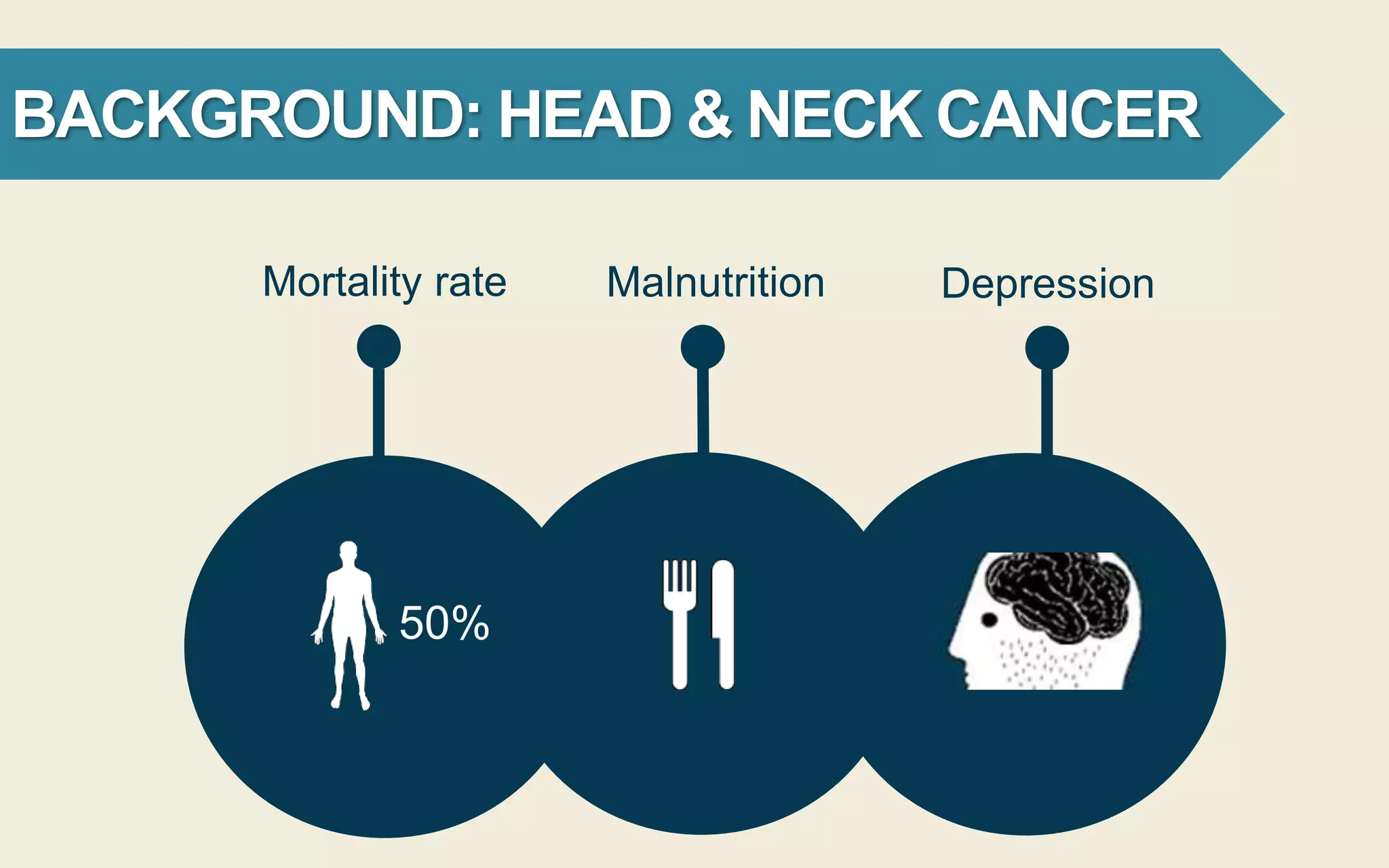

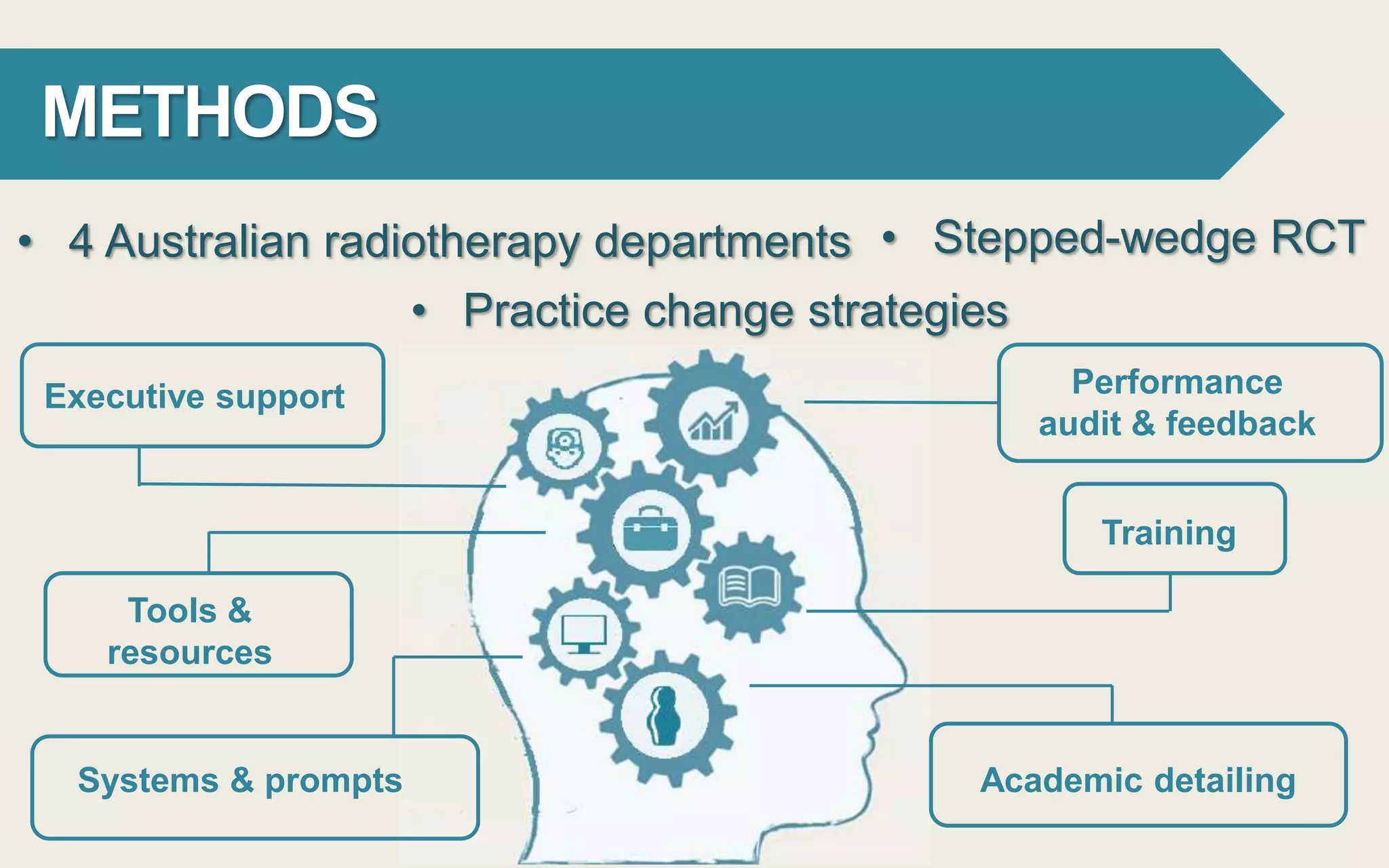




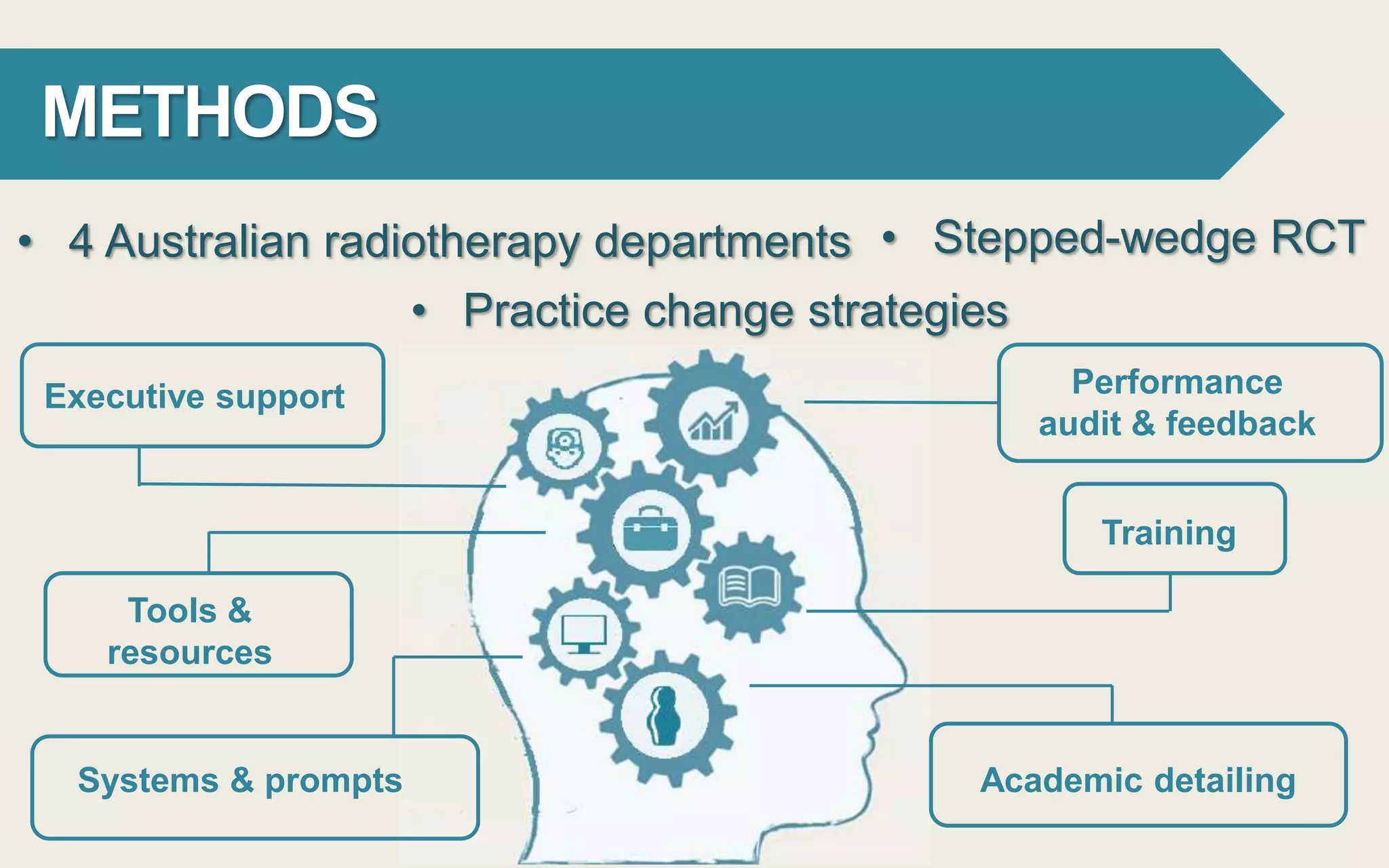
This document outlines a clinical practice change aimed at enhancing dietitian screening for depression and referrals for psychosocial support in head and neck cancer patients across four Australian radiotherapy departments. The intervention involves performance audits, training, and resources, with initial results showing no patients screened during the control period. If successful, this model could improve guideline implementation and health outcomes for numerous patients both nationally and internationally.