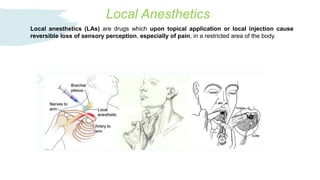
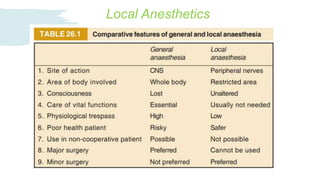
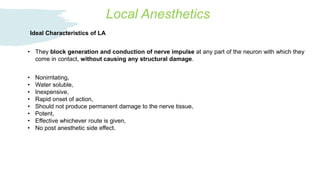
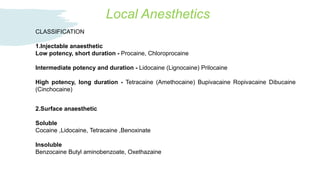
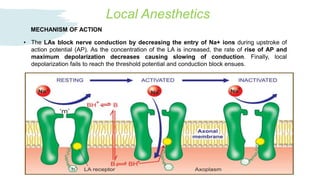
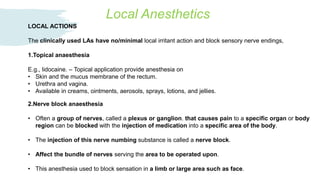
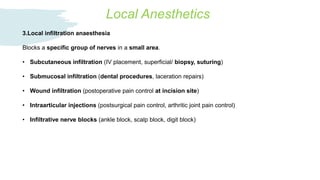
Local anesthetics reversibly block nerve conduction, providing numbness in a localized area. They work by decreasing sodium ion entry during the action potential upstroke, slowing and eventually blocking nerve conduction. Common local anesthetics include lidocaine, bupivacaine, and tetracaine. They can be administered via surface application, nerve block, local infiltration, or regional techniques like spinal or epidural injection to provide anesthesia for procedures. While generally safe at correct doses, overdose can potentially cause adverse effects involving the central nervous system, cardiovascular system, or hypersensitivity reactions.