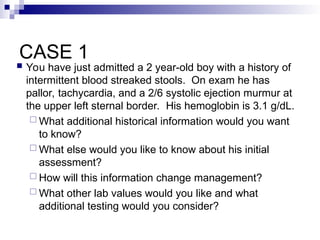
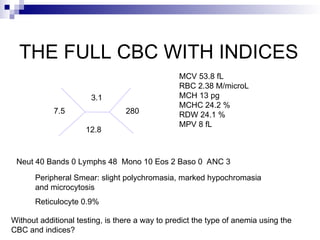
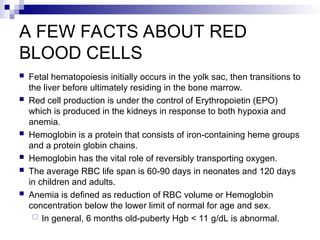
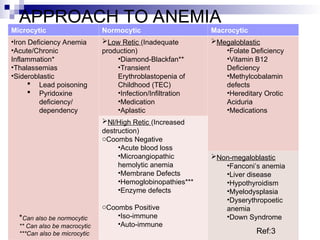
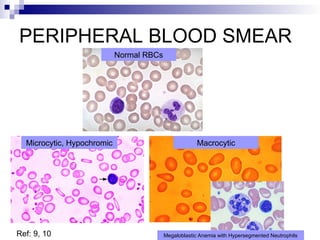
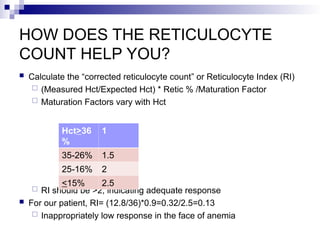
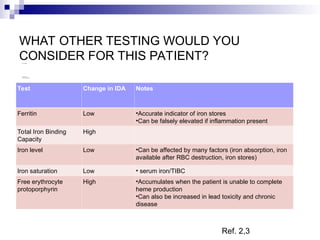
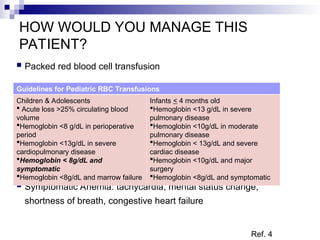
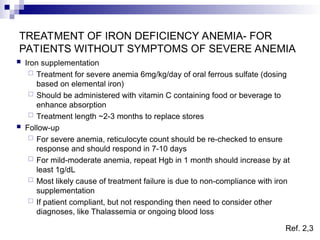
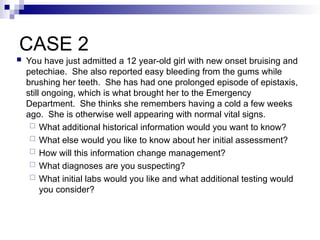
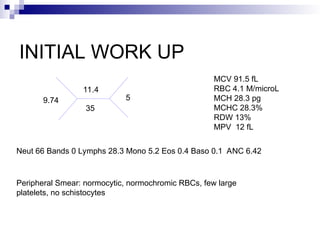
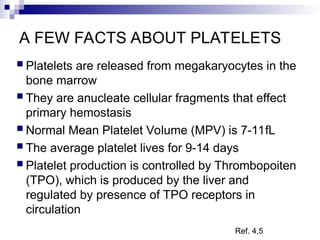
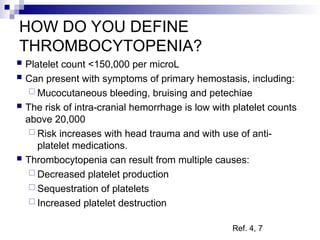
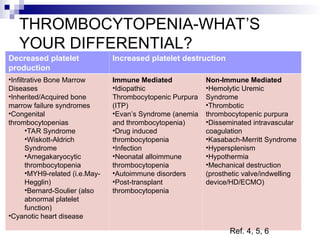
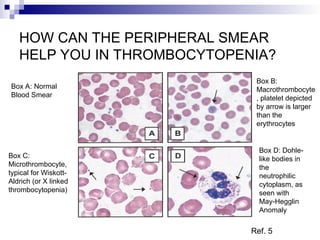
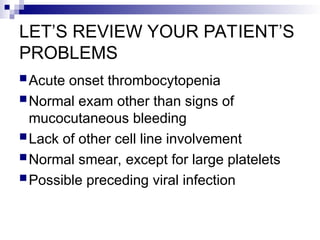
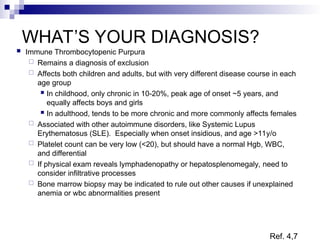
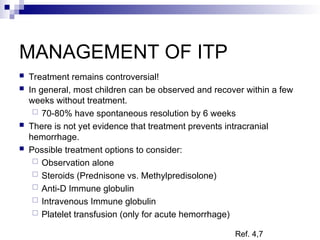
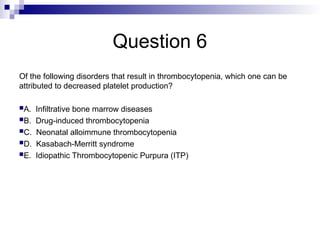
The document discusses pediatric abnormal complete blood counts (CBC) focusing on anemia and thrombocytopenia. It presents case studies to illustrate diagnostic approaches, including required historical information, laboratory evaluations, and management strategies. Key learning objectives include identifying CBC abnormalities, formulating differential diagnoses, and recognizing the need for further studies in abnormal cases.