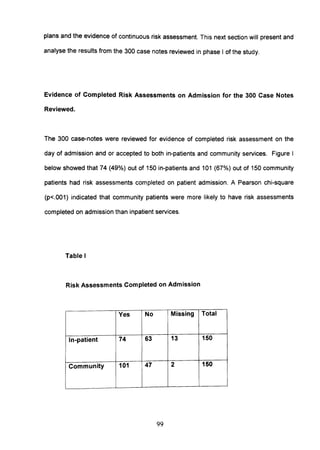
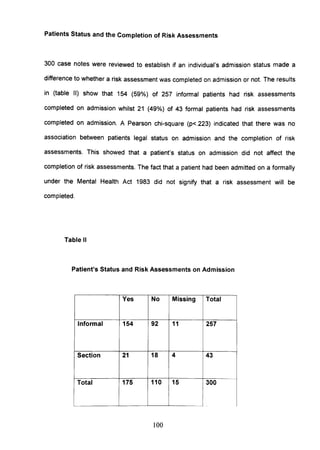
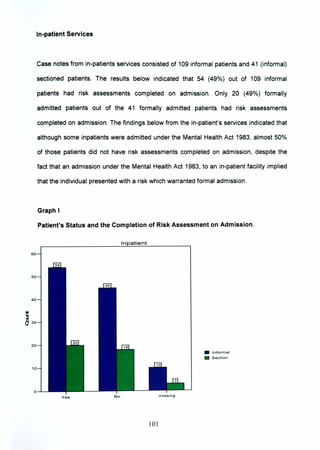
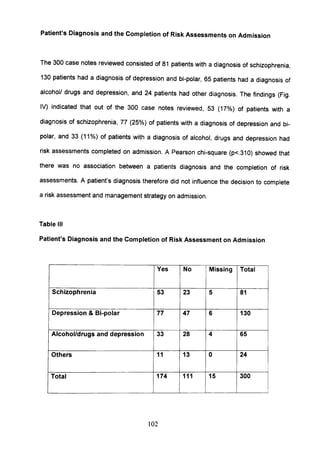
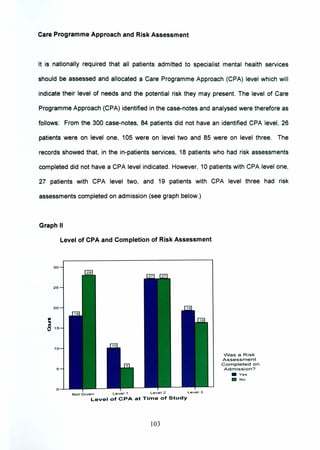
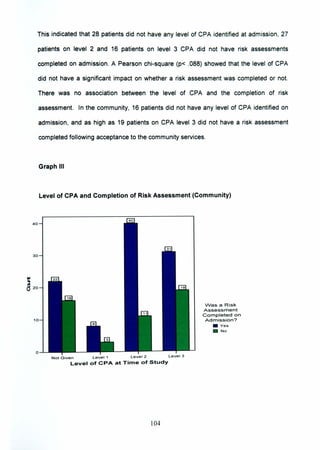
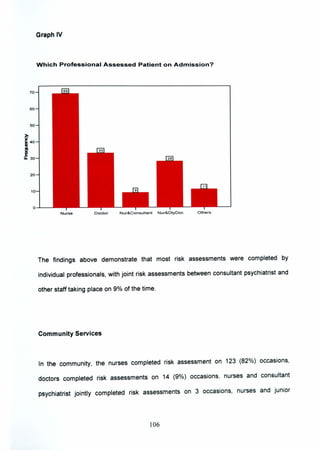
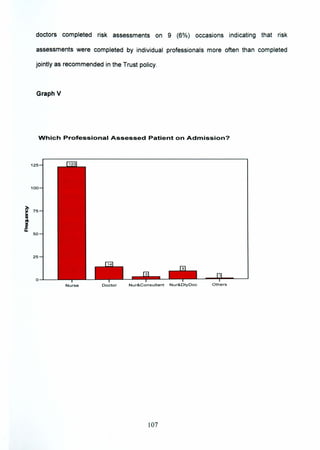
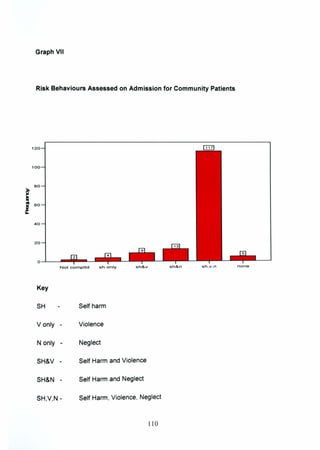
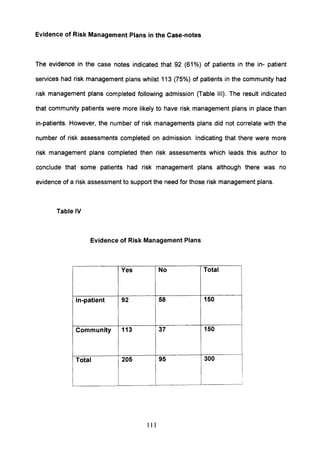
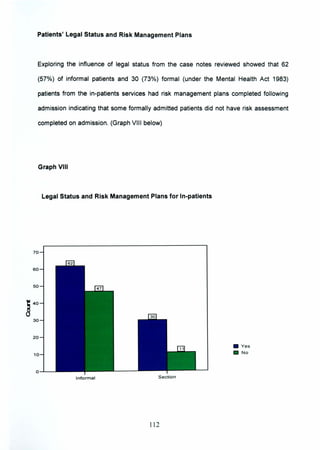
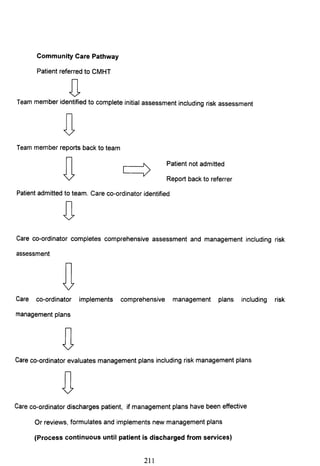
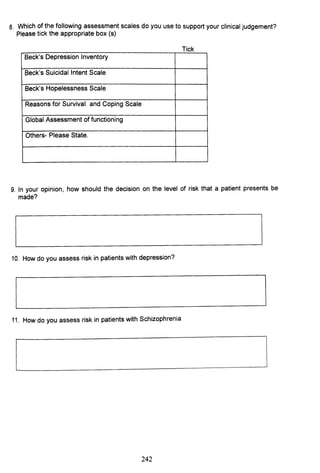
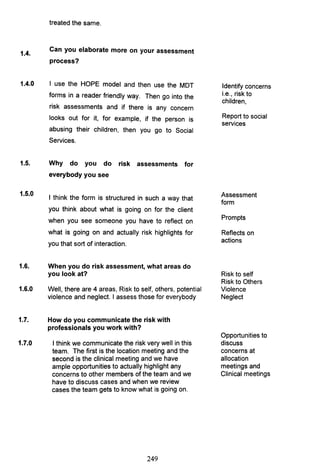
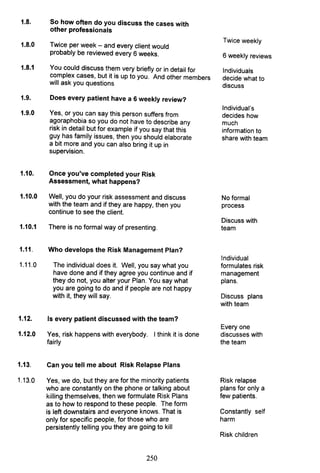
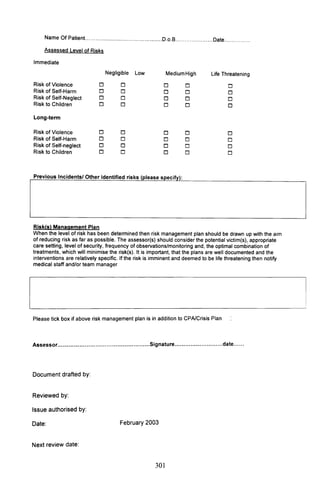
This document summarizes a doctoral thesis that investigated how nurses manage risk presented by people with severe mental health problems. The study used a mixed-methods approach including a review of 300 case notes and interviews with 10 UK nurses and international experts. The case note review found inconsistencies in risk assessment documentation. Interviews revealed varied risk assessment practices among nurses and perceptions of a "blame culture" hindering documentation. Experts in the US perceived standardized risk assessment tools and team-focused care as protective against litigation. The study aims to make recommendations to improve nursing risk assessment training and accountability.