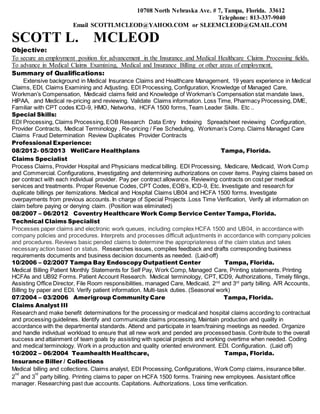
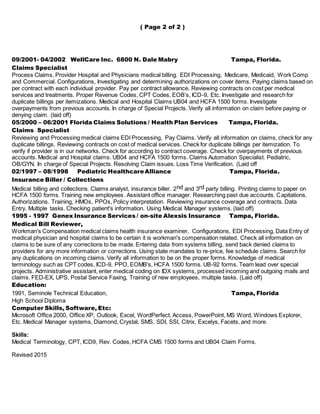
Scott McLeod is seeking a position in insurance or medical claims processing with over 19 years of experience processing various types of medical claims including workers compensation, Medicare, Medicaid, and commercial insurance. He has extensive experience with EDI processing, claims examining, adjusting, and researching as well as managing provider contracts and understanding various coding systems. The resume provides a detailed employment history of his medical claims and billing roles with various insurance companies and healthcare providers.