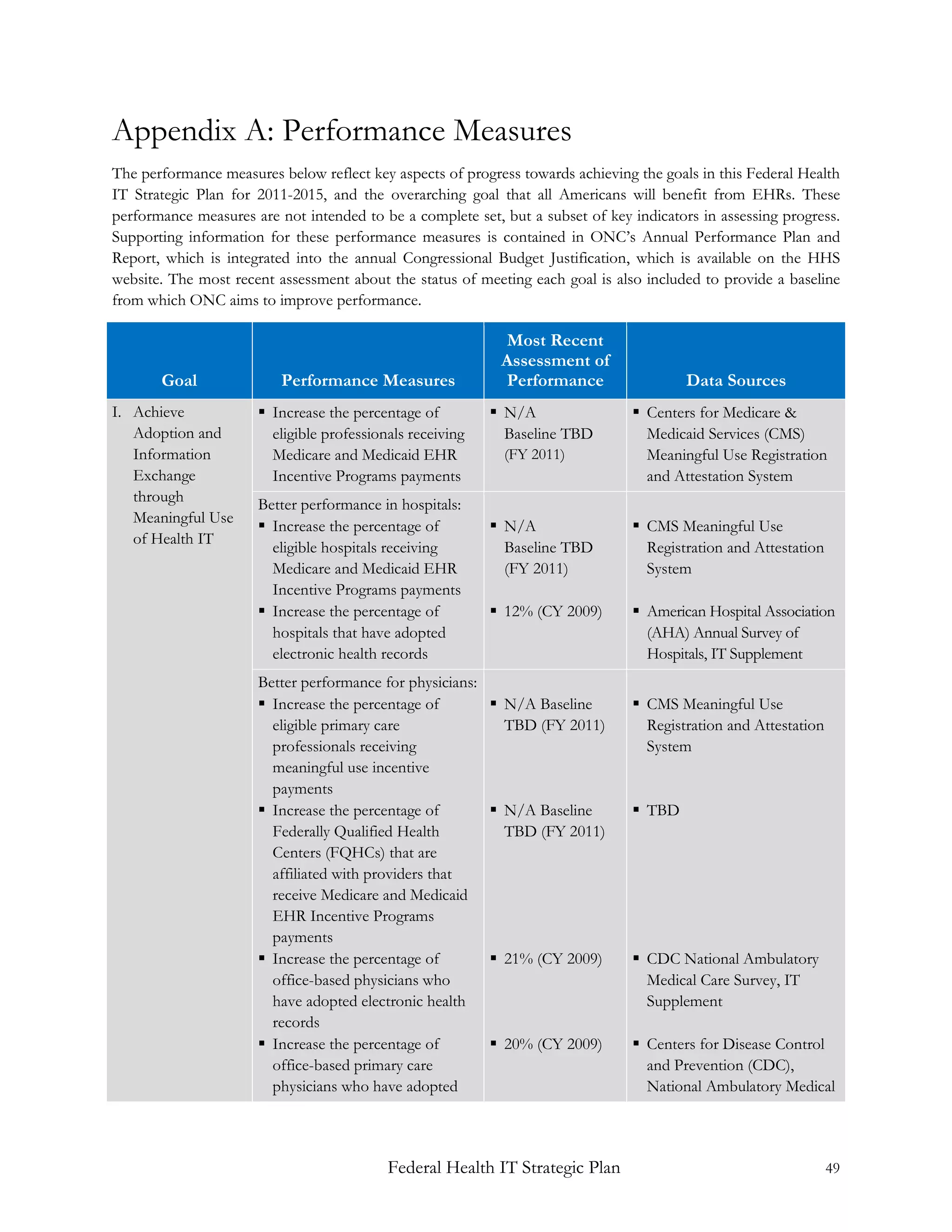
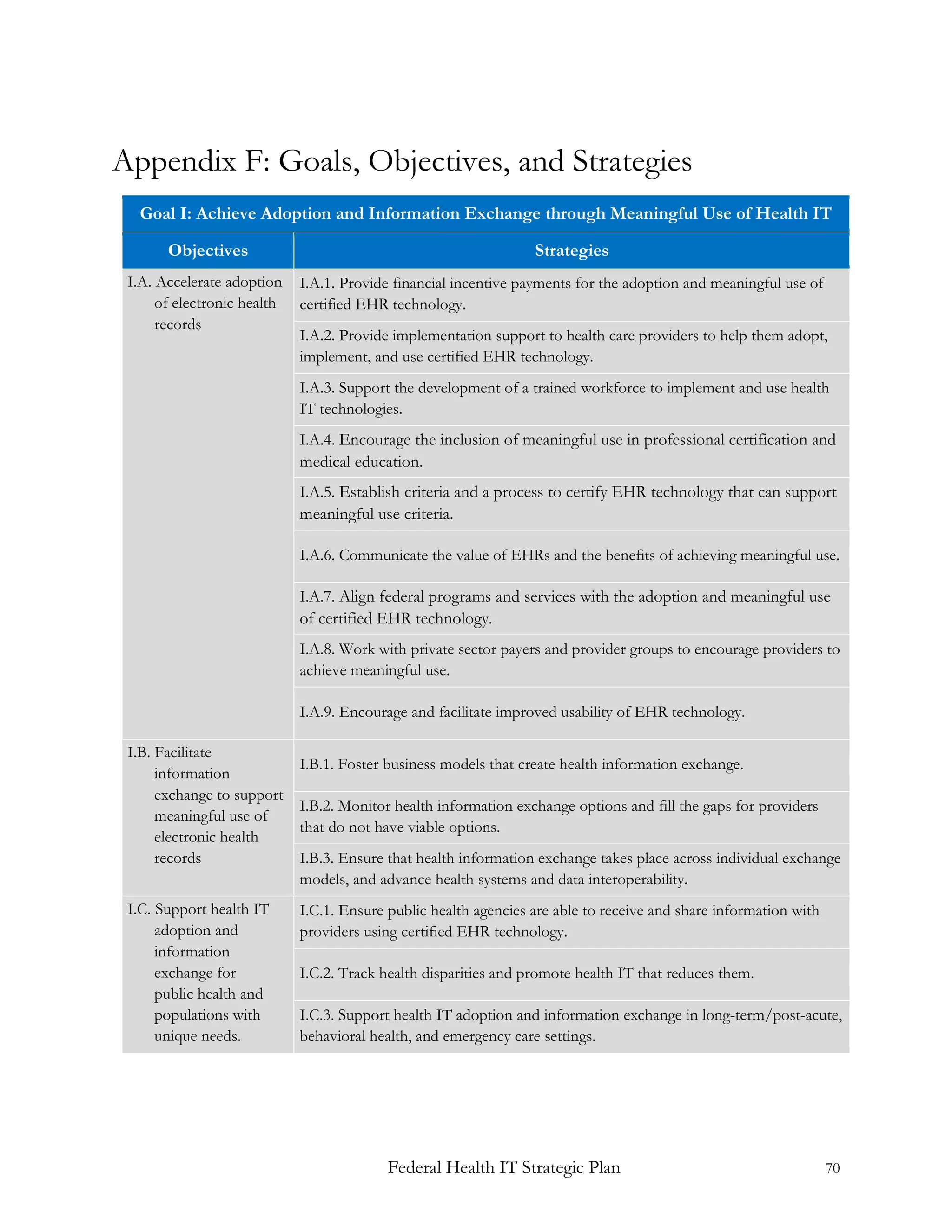
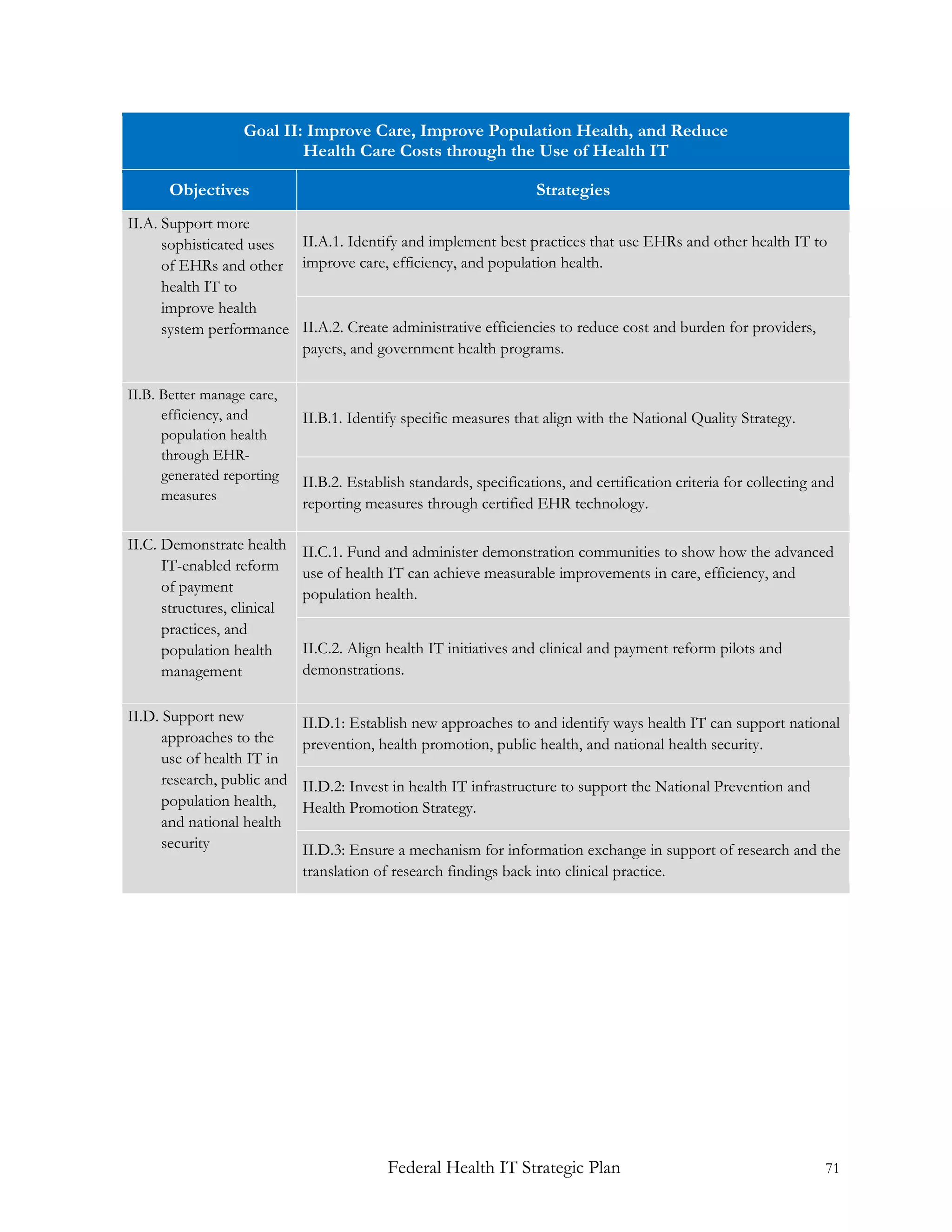
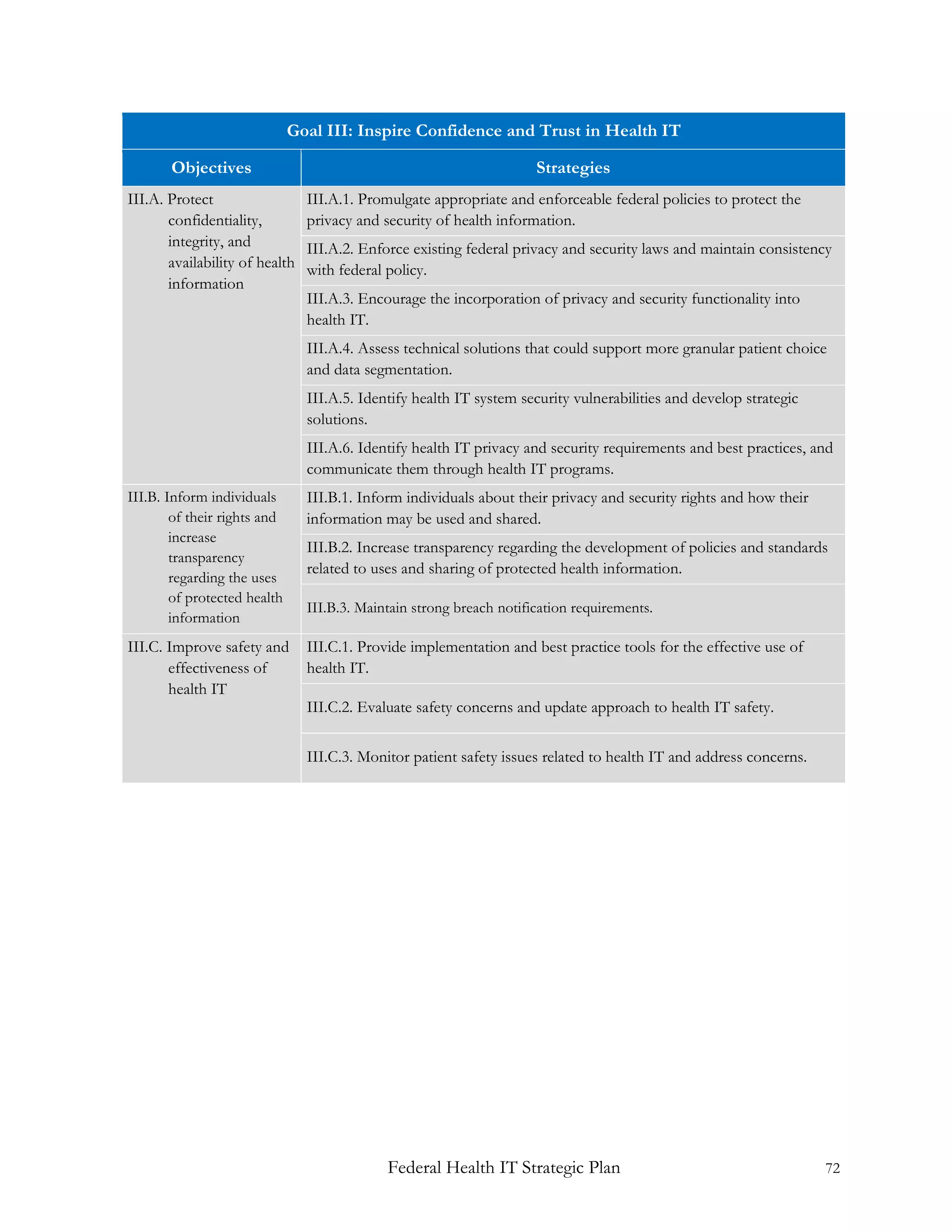
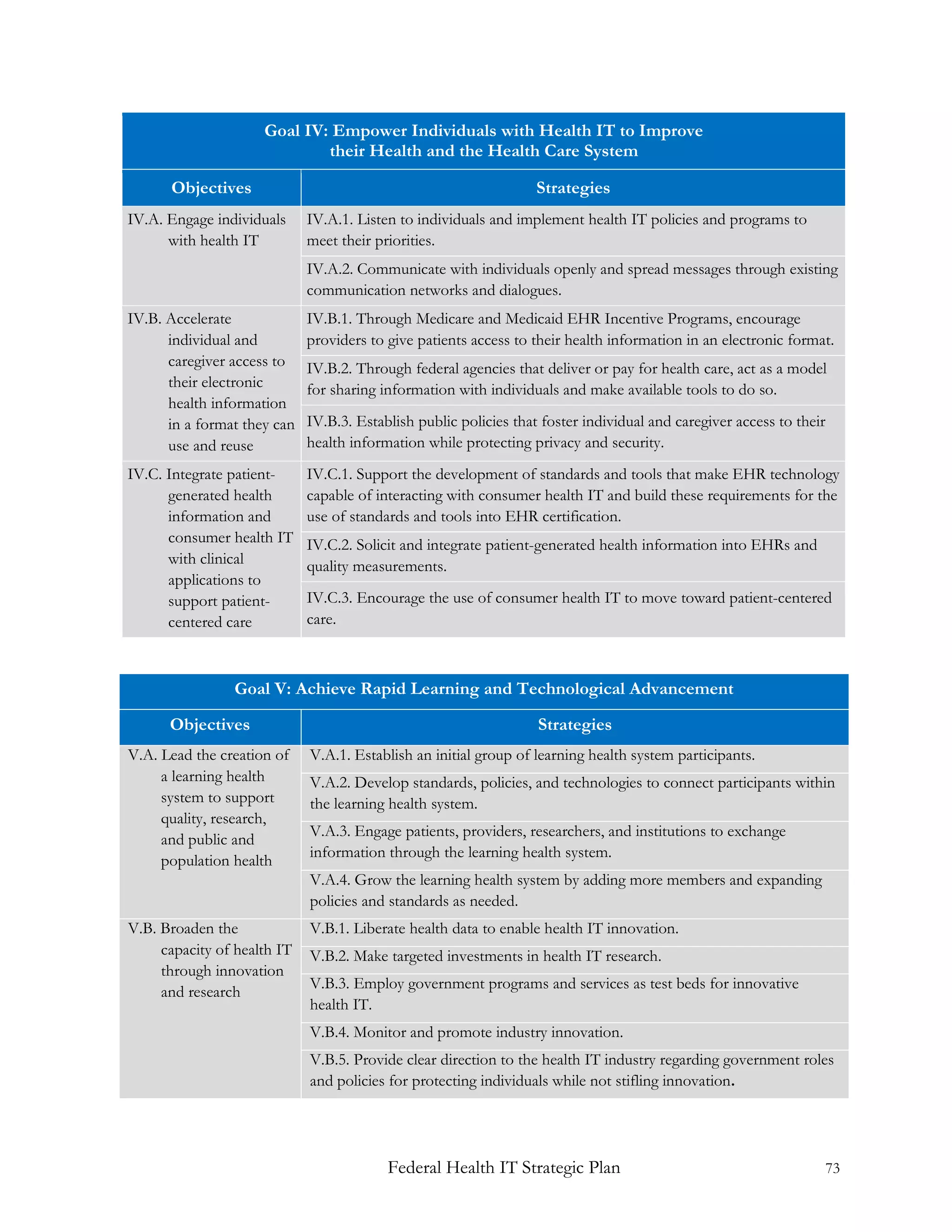
The Federal Health Information Technology Strategic Plan 2011-2015 outlines a framework to enhance health IT adoption and information exchange to improve health care outcomes for all Americans. Key goals include promoting meaningful use of electronic health records (EHRs), improving population health while reducing costs, and ensuring trust in health IT through improved privacy and security measures. The plan recognizes the necessity of innovative approaches to support individual health empowerment and the efficient integration of health IT into everyday healthcare practices.