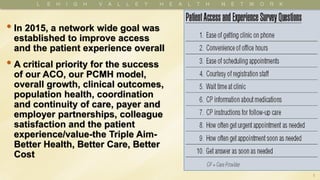
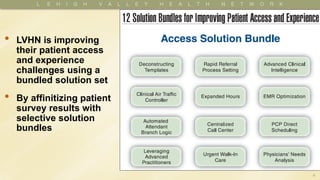
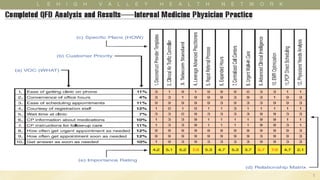
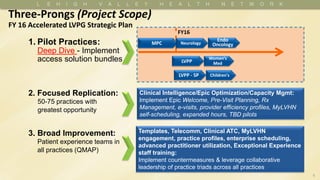
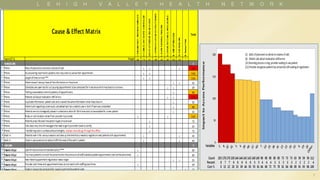
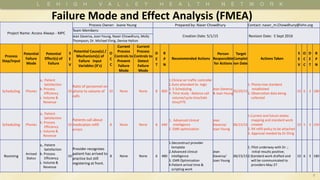
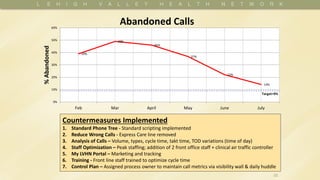
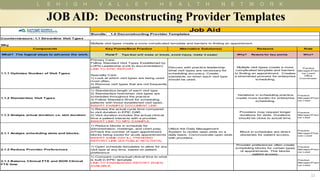
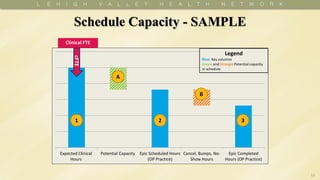
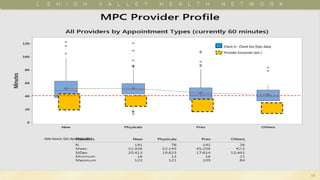
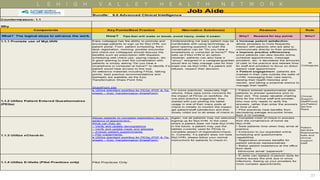
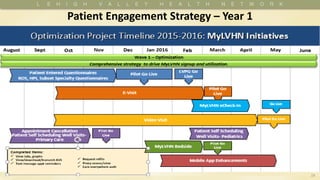
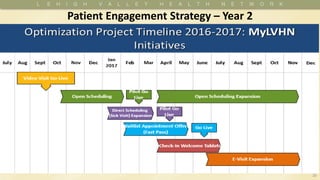
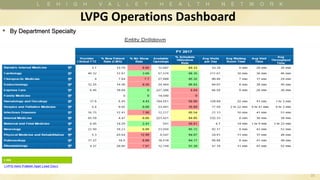
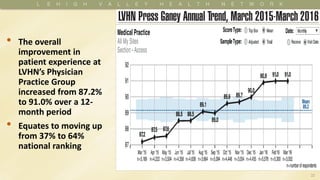
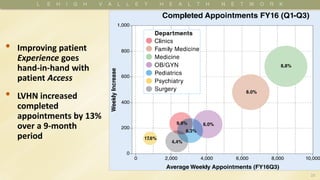
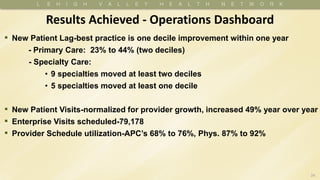
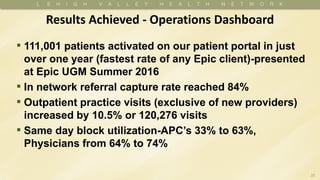
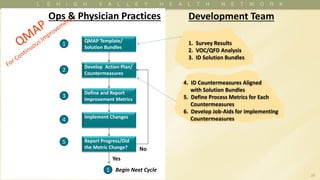
LVHN has improved patient access and experience using bundled solutions. They analyzed patient survey results to identify solution bundles to implement countermeasures. This included standardizing provider templates, promoting the patient portal, utilizing clinical intelligence and optimizing the EMR. As a result, patient experience scores increased from 87.2% to 91% nationally, completed appointments increased 13%, and 111,001 patients were activated on the patient portal, the fastest rate of any Epic client. LVHN continues using a plan-do-study-act cycle to implement changes, measure metrics, and report progress.