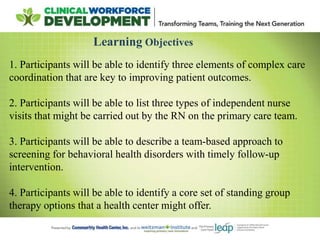
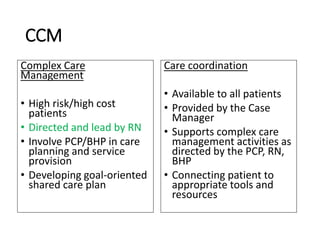
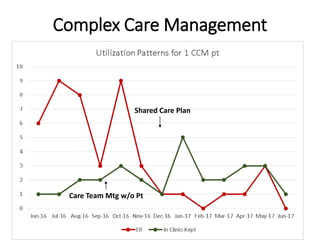
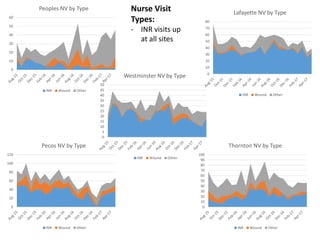
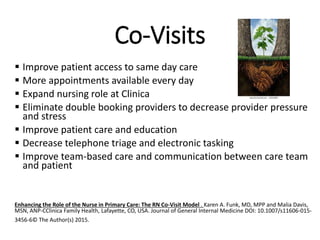
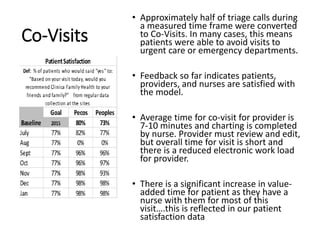
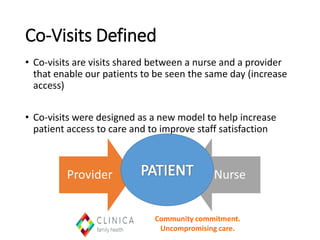
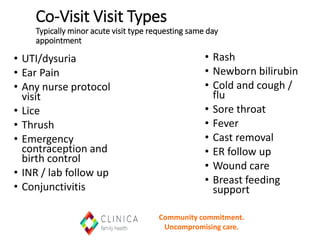
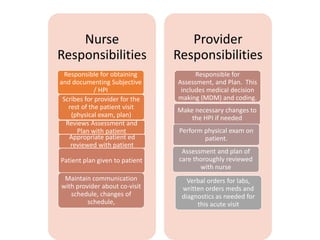
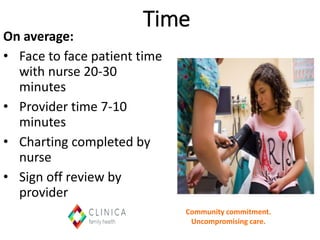
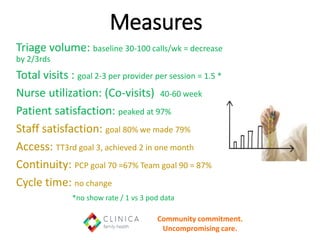
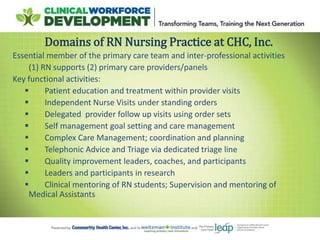
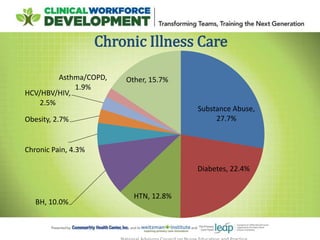
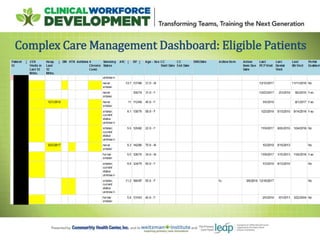
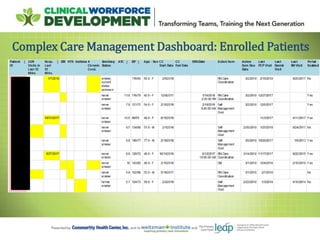
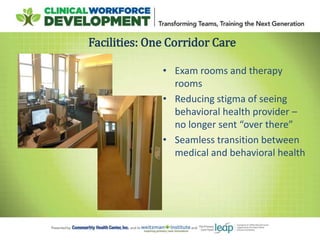
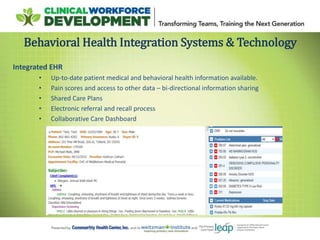
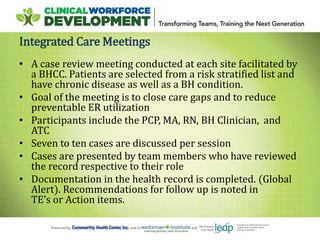
The document discusses expanding the role of registered nurses (RNs) in primary care settings. It describes how RNs can take on responsibilities like complex care management, active schedule management, using data to monitor patient outcomes, and conducting co-visits with providers to increase access to care. Co-visits allow RNs to address minor issues while providers briefly review cases. The approach has led to improved access and patient satisfaction at Community Health Center, Inc.